8.07 Safe Exercise
Presented by: Dr Jo Preston, Dr John Brooks (GP), Ananthi Puntis (Physiotherapist)
Faculty: Dr Iain Wilkinson, Dr Alice O’Connor
Broadcast Date: 5th November 2019

Social Media
Spotted by Ananthi Puntis:
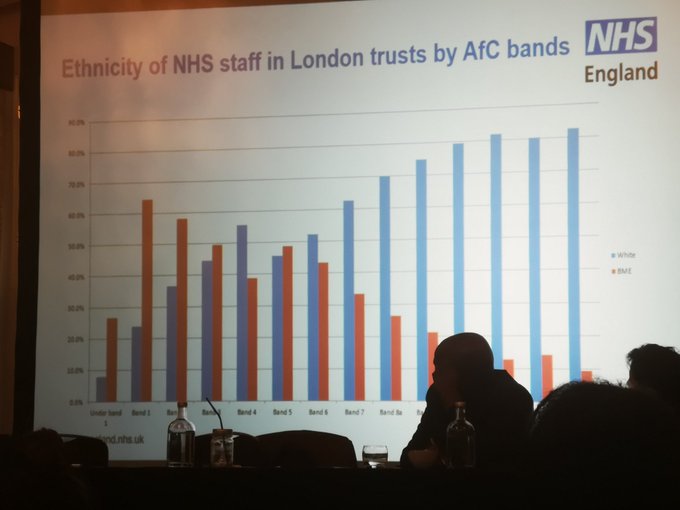
Tweet from Abdullah Mia (@mianthrope) of a graph showing NHS staff by ethnicity and banding. Shocking!
Learning Outcomes
Knowledge
- To appreciate the health benefits of exercise and the evidence base for this
Skills
- Identify specific situations in which physical exercise or activity may need to be limited
Attitudes
- To weigh the balance of benefits versus risks of exercise.
CPD Log
Show notes
Definitions
Formal Definition
What we’re actually encouraging is physical activity rather than just exercise. Just getting people moving. Talking about exercise (and sport) can have negative connotations for many patients
Physical activity: Any bodily movement produced by skeletal muscles that requires energy expenditure. Includes a broad range of activities: Everyday activities (walking, climbing stairs, carrying children), Household chores, Occupational tasks, Leisure time physical activity, Exercise
Exercise: Physical activity that is planned, structured, repetitive, and purposeful (aimed at improving or maintaining one or more components of physical fitness). Includes: Walking, Swimming, Cycling, Aerobics, Yoga, Tai Chi, Strength exercise, Cardiac and pulmonary rehabilitation, Falls prevention exercise classes
Energy expended is a product of FITT:
- Frequency
- Intensity (effort)
- Time
- Type
Physical fitness: A set of attributes that people have or achieve that relates to the ability to perform physical activity.
Types of physical fitness: Cardiorespiratory endurance, Muscular strength, Balance and coordination, Flexibility. Influenced by genetics, health conditions, physical activity and exercise (cause adaptations that have multiple health benefits)
Main Discussion
Why are we doing this episode?
Physios have knowledge of what will happen with the exercise session/ class, but may not feel that they have enough back-up knowledge of the physiology to feel safe deciding whether or not the intervention you are providing may cause harm, particularly in a multimorbid population.
This episode is about trying to provide some of that information so that you can feel more comfortable with deciding who may need medical clearance, as well as a better understanding of the risk vs benefit of exercise.
Responsibility:
- Whose responsibility is it to say someone is safe to exercise? The physio delivering the exercise or a doctor who knows the patient?
- Asking GP for clearance often delays therapy, and may not gain an accurate opinion dependent on their knowledge of the patient.
Why is exercise good?
See physical activity as a modifiable risk factor
Importance of exercise
- Benefits in terms of reducing comorbidities including dementia etc.
- Reduction in all-cause mortality (increased lifespan, helps reduce the risk of dying early) (37,000 premature deaths could be prevented annually in the UK)
- Improved health: reduced risk of multiple non-communicable diseases so living a healthy longer life. Including type 2 diabetes (35-50%), cardiovascular disease (20-35%), hypertension, cancer (colon, breast and endometrial) (20-50%)
Physical activity/ fitness needs to be current to maximise the effects.
Age is irrelevant, benefits can still be gained at any age.
It is also (potentially)
- Cheap, with indiscriminate benefits (>20 conditions)
- Independent of other risk factors
- Minimal side-effects.
- Chief Medical Officer called it a “wonder drug”
Some relevant links:
https://www.csp.org.uk/networks-campaigns-influencing/campaigns/love-activity-hate-exercise
https://www.csp.org.uk/public-patient/keeping-active-and-healthy/how-get-more-active
The Miracle Cure https://www.bmj.com/content/366/bmj.l5605
Specifically in older adults:
Falls prevention
- The problem: ~30% fall each year (70% cause injury, 35% have a decline in function) 66% fall again within 1yr
- Falls risk reductions with home or group exercise programmes: Rate of falls 40% lower, Rate of injurious falls 41% lower.
- Examples: Falls Management Exercise FaME, AgeUK: Falls prevention and keeping active, Otago Exercise Programme
- Balance and strength training includes weights so will increase cardiac output etc.
- Falls prevention classes are not standardised across the country: run by public health, physios or exercise instructors. Criteria for inclusion may vary e.g. blood pressure, TUG, low level vs high level.
- Other benefits: general wellbeing, maintenance of independence, improved mood, reduced risk of dementia, joint and back pain improved, social aspects.
Guidelines:
- 150 minutes of moderate intensity activity (breathing fast but still able to talk) or 75 mins of vigorous intensity (breathing fast, difficulty talking) exercise (or a combination of moderate and vigorous intensity) spread across the week.
- Muscle strengthening activities at least 2 days of the week (can be exercising with weights, carrying shopping, gardening, yoga, gym)
- Elderly: balancing 2 days of the week to reduce risk of falls and increasing independence (dance, bowls and Tai Chi)
- Minimise the amount of time spent sitting (sedentary) for extended periods (break up periods of inactivity)
So why is this more of a worry with older adults than, say, younger adults with heart and lung problems?
There are changes to the normal physiology as we age, such as reductions in:
- VO2max
- Strength
- Flexibility
- Proprioception
- Muscle mass
- Mobility
These are all associated with sedentary behaviour but all preventable and reversible with physical activity/ exercise.
We therefore need to keep older adults as active as possible for as long as possible.
Practical simple clear messages:
- Be active
- Sit Less
- Build Strength
- Improve balance
- The more you do, the greater the health benefits
Simple ways to achieve this include the use of pedometers and apps including SGH Pace-up trials (Tess Harris) & activity monitor (sitting or standing).
Step counts often don’t measure intensity, but there is emerging evidence that increased step count can lead to reduced all-cause mortality risk
Other considerations:
- What do you enjoy doing (job, leisure, family)? Can you do a bit more?
- What have you done in the past? (remember negative experiences of sport at school)
- Goals and potential benefits (playing with grandchildren, reducing risk of further illness)
- Sit less, move more, don’t take it easy in retirement!
- Find opportunities to be active
So what’s the harm?
Common fear amongst patients and healthcare professionals: I’m going to cause harm by exercising/ getting someone to exercise.
Stats on how unlikely you are to die when exercising:
- Risk during exercise is ~1 sudden death per 1.5 million episodes of exertion. Albert, C. M., M. A. Mittleman, et al. (2000). New England Journal of Medicine 343(19): 1355-1361
- Physical activity may slightly increase risk of cardiovascular event during exercise if CVD risk factors are present… but it doesn’t necessarily stop someone exercising.
- Physical activity decreases risk of a cardiovascular event & premature death in the future.
- It is the disease not the exercise that kills people in these circumstances (exercise is the trigger). In the longer term, there is more overall benefit on QOL and mortality from doing exercise.
Long-term risk to health of NOT exercising is much higher!
You can reduce the risk of musculoskeletal injury and cardiovascular events by
- Injury prevention warm-up programme (FIFA 11+)
- Warm-up (15 mins) & cool-down (10 mins each) BACPR 2008
- Start @ low intensity & build up
- 10 minute bouts of physical activity in elderly
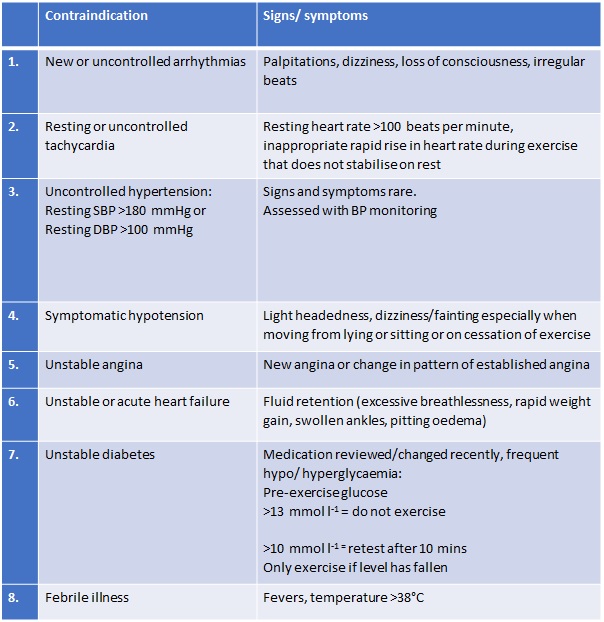
Recognised relative contraindications to exercise: (These are for use in community settings, rather than for superceding clinical judgement.)
BACR (2006) Phase IV Exercise Instructor Training Manual and ACSM (2009) Guidelines for Exercise Testing and Prescription
Stop exercising and contact GP/ A&E as appropriate if unusual or unexplained or if doesn’t resolve at rest:
- Chest pain
- Shortness of breath
- Dizziness/ light-headedness
- Other unexplained symptoms
NERD ALERT
Effects of some common medications on exercise:
ACE-I & ARBs:
- ↓ peripheral resistance = risk of postural hypotension due to blood pooling
- ↑susceptibility to dehydration (& postural hypotension, DO NOT limit maximal O2 uptake)
β-blockers:
- ↓ cardiac rate & output: attenuated normal physiological response to exercise
- Lack of tachycardia disliked (no “adrenaline like response”) + restricted exercise capacity in endurance events
- Possible adverse effects: postural hypotension, excessive tiredness, (potentially) masking hypoglycaemia in diabetic patients.
- Unsure if as beneficial for health if limits them to the extent that they can’t exercise to a higher intensity?
- Angina patients: usually able to tolerate more exercise without symptoms
Diuretics:
- Risk of dehydration causing postural hypotension:
- Remain hydrated but don’t get overloaded!
- Avoid prolonged standing after exercise
- Avoid taking before exercise
Calcium channel blockers & nitrates (inc. GTN)
- Impair cardiac output = reduced exercise capacity
- Peripheral vasodilation = venous pooling & postural hypotension (esp. during cool-down)
- Adverse effects balanced with drugs ability to improve exercise tolerance by improving blood flow to heart
Adaptations in physiology, in the longer term
There are hundreds of adaptations, but here are some examples:
Cardiorespiratory training:
Physiological adaptations include: ↑ capillaries, ↑ mitochondrial number, size & function, ↑ GLUT-4 number & translocation & ↑ lipoprotein lipase on capillary endothelium
Functional consequences include: ↑ cardiorespiratory fitness and ↑ endurance capacity (maintain exercise for longer)
Health consequences include: ↑ HDL cholesterol & ↓ VLDL and LDL cholesterol , ↑ glucose uptake and metabolism
Resistance training:
Physiological adaptations include: ↑ motor unit recruitment and improved coordination of recruitment
Muscular adaptations include: hypertrophy
Functional consequences ↑ strength (25-100% ↑ in a few months)
E.g. Aim of exercise is to induce ischaemia in tissues in claudication to promote localised adaptation, for example allowing greater oxygen delivery through increased capillary density.
Training principles that influence adaptations:
- Specificity of training performed
- Progressive overload
- Reversible & transient (within days)
- Individual response (trainability) (including genetics and health status)
In summary we’ve seen
- The positive benefits of exercise
- The low risk of cardiac death
- The negative effects of not exercising
We all need to be encouraging older adults to exercise: every encounter counts. We should aim to contribute to the changing mindset of ‘convalescence’. Overly protective measures can limit people’s independence.
Curriculum Mapping
NHS Knowledge Skills Framework
- Core 2 Level 1
- HWB1 Level 1
- HWB4 Level 2
- HWB7 Level 2
Foundation Programme
- Sec 1:4 Self directed learning
- Sec 2:6 Interface with HCPs
- Sec 3:10 Frail pt
- Sec 3:10 Support for pts
- Sec 3:16 (all)
- Sec 3:18 (all)
GPVTS
- 3.05 Clinical management – local rapid access referral pathways, physical factors,including exercise, that disproportionately affect the health of older people, support services for older patients
- 3.05 Managing medical complexity – be able to promote health on an individual basis, understand the ability of an elderly person to carry out all the activities commensurate with their mental competence
- 3.05 Maintaining performance, learning and teaching
- 3.05 Practising holistically and promoting health – Know the preventative strategies required in the care of older people
Core Medical Training
- Managing long term conditions and promoting patient self-care: Rehabilitation and MDT, Quality of life
- Health promotion and public health: Factors affecting health, Lifestyle
- The Top Presentations: Falls
- Other Important Presentations: Immobility, Unsteadiness / Balance Disturbance
- Geriatric Medicine: MDT assessment, Rehabilitation targets, Preventative approach, Deterioration in mobility, Falls
Geriatric Medicine Specialty Training
- Managing long term conditions and promoting patient self-care: Rehabilitation and MDT, Quality of life
- Health promotion and public health: Factors affecting health, Lifestyle
- 29. Diagnosis and Management of Chronic Disease and Disability
- 30. Rehabilitation and Multidisciplinary Team Working
- 35. Falls
- 36. Poor Mobility
- 40. Community practice




