7.06 Falls: to admit not not?
Presented by: Dr Iain Wilkinson, Dr Jo Preston, Sarah Smith and Alison Fitzgerald.
Broadcast date: 23rd April 2019
Learning Objectives
Knowledge:
- Recall common causes of falls in older adults
- Distinguish causes for which acute admission may modify outcome
Skills:
- Be able to recognise when acute admission is necessary in someone who has fallen
- Recognise when falls review in the community may be beneficial
Attitudes:
- To appreciate that falls risk can often never be abolished completely
Social Media This Week
Iain:
Building from tacit & tribal knowledge for better leadership -> requires Narrative + Engagement + Technology — NET Framework.. https://t.co/ki9nycCB5p @julianstodd pic.twitter.com/gnz6pKnh1x
— Edouard Legoupil (@edouard_lgp) March 11, 2019
Here is the blog article: https://julianstodd.wordpress.com/2013/08/19/the-net-model-for-social-leadership/
Jo:
https://journals.sagepub.com/doi/full/10.1177/0141076816646944
Main Show Notes:
Definitions:
Focus of episode: to explore the reasons that a person may need to be admitted following a fall. In the main this means admission to an acute trust but may mean ‘admission away from home’ i.e. a community bed.
The decision between the two, versus staying at home depends on the availability of certain treatments and members of staff for management and as such will vary depending on your local provision. For example, some community hospitals will do intravenous infusions, others may not, some hospital at home services may be able to provide this. So there are no hard and fasts but we’ll explore the main principles to help you be able to make informed decisions with your patient.
Key Points from Discussion
This episode links with:
The prevalence of gait disorders increases from 10 % in people aged 60-69 years to more than 60 % in community dwelling subjects aged over 80 years.
Gait disorders in adults and the elderly – A clinical guide by Pirker & Katzenschlager in The Central European Journal of Medicine 2016
- Human gait depends on a complex interplay of major parts of the nervous, musculoskeletal and cardiorespiratory systems.
- The individual gait pattern is influenced by age, personality, mood and sociocultural factors.
- With advancing age the proportion of patients with multiple causes or combinations of neurological and non-neurological gait disorders increases.
People can be thought of as complex biological symptoms, well functioning systems can handle a variety of different stressors without breaking down. Older people who are frail can be thought of as a complex system that struggles to adjust to many small stressors which people who are not frail would find innocuous. A fall can be thought of as a manifestation of a system that is struggling to optimally function, a fall is often then the first presentation of a frailty crisis as walking is a complex activity requiring coordination between multiple different body systems.
We are going to structure this episode by using a head to toe approach to the causes of falls, looking at acute and chronic causes of falls at each stage. Bearing in mind that in older adults, the likelihood of multifactorial causes for falls increases.
Vision & Vestibular
Afferent nerves from the visual, vestibular and proprioceptive systems provide essential information on the position of the body and its parts. Disturbances in one of these systems, e. g. proprioception, may be partially compensated by other sensory systems, such as vision.
Eyesight:
More likely to be a long term issue than acute. Examples of acute visual disturbance:
- Occipital or retinal stroke: needs acute assessment as inpatient
- GCA: needs acute assessment but often ambulated after initial assessment
- Acute angle closure glaucoma: ophthalmological emergency.
Will cause reduction in visual field / depth perception eg. as well as potential decompensation of above.
Chronic causes can be exacerbated by concomitant delirium
- Cataracts: signpost to GP if not already known – surgery reduces risk of falling
- Macular degeneration – if rapid consider wet AMD
Will often have compensated their environments and routines over time.
Balance:
Vestibular system particularly prone to dysfunction in older adults (ep 1.09 – Dizziness) both chronic and acute.
Acute causes:
- BPPV: Epley manoeuvre and OPD management – ability to function at home will be the determinant here (as below).
- Acute labyrinthitis: OPD management usually.
- Cerebellar or brainstem stroke affecting eye movements or cerebellar function: acute inpatient management.
Chronic causes of dizziness are more likely to be due to a combination of disruption at a number of points on the pathway between visual, vestibular, proprioceptive and central, processing and psychological: unlikely that acute admission will alter this but seemingly small triggers may make it seem unmanageable at home. From a medical perspective, unless there is a treatable trigger, it is unlikely that admission will improve things. However, physiotherapy to improve confidence and look at functional support is often helpful but early assessment is needed to determine this.
Brain / CNS
Afferent information from visual, vestibular and proprioceptive systems are received in the brain, interpreted and processed to provide signals to the body to move.
This involves many areas of the brain including
- Frontal cortex – important for executive function e.g. task planning, motor cortex is here
- Basal ganglia – control of movement
- Brainstem – reflexes
- Cerebellum – control of coordination
Safe walking requires intact cognition and executive control. Acute onset of a gait disorder may indicate a cerebrovascular or other acute lesion in the nervous system but also systemic diseases or adverse effects of medication, in particular sedatives.
Parkinsonism and frontal gait disorders due to subcortical vascular disease or disorders associated with dementia are among the most common neurological causes.
Acute Dysfunction
- Stroke in any of those areas: will be associated with other focal signs
- Delirium often disrupts these complex pathways in a variety of ways: decision re admission then related to both whether the underlying precipitant can be treated outside of hospital as well as whether support for the consequences on mobility and cognition can be.
Chronic Dysfunction
- Dementia
- Parkinson’s Disease
Psychological:
Fear of falling, anxiety, low mood e.g. motivation, pain.
Moving further down the pathway from brain to limbs: the efferent system comprises descending pathways including the pyramidal tract, peripheral nerves, neuromuscular end plate and muscles.
- Pyramidal tract (motor pathways) signs might be seen in stroke (new or old), spinal cord compression.
- Neuromuscular disease is usually chronic and reasonably rare e.g. MND, polymyositis: management for most of these occur as an outpatient even though they are serious conditions so again, comes down to functional ability
Musculoskeletal
Hip and knee osteoarthritis are common non-neurological causes of gait disorders.
Joint stability:
Usually long term vs injury – directly related to sarcopenia plus OA and other chronic conditions. Pain is most likely to be the limiting factor in chronic joint conditions and may require admission to optimise e.g. steroid for RA, analgesia to facilitate weight bearing. If sudden onset and related to a fall, may need to assess for fracture or ligament damage.
Sarcopenia:
Poor strength and muscle mass, relation to nutrition: have they the support to get nutrition?
Growing evidence that you can build muscle mass plus 70 – exercise is the single thing that can be improved and impact on falls prevention
Cardio-pulmonary
Breathlessness due to either may limit exercise tolerance and therefore enter a cycle of decline through deconditioning.
Admit if:
- low oxygenation as cause of breathlessness
- Suspected arrhythmia as cause of fall (sudden, unprecipitated collapse) – will need usually 24 hours cardiac monitoring: fix is a pacemaker / medication.
Postural hypotension with symptoms: 1 in 5 community dwelling older adults have a postural drop so symptoms are the important factor here – if it is acute onset, it will usually be associated with symptoms. Not all need admitting though – function and safety the determinants (ep 6.02)
Continence
Continence impacts falls and falls (mobility) impact continence.
- If urinary incontinence is new then consider if it might be a UTI – note new PHE guidance on not using dipsticks. Outpatient management unless sepsis, dehydration needing iv fluids, or functionally affected.
- New faecal incontinence: check for overflow (common cause), check for associated neurology to suggest spinal lesion. Latter needs inpatient management, former does not.
Feet
Sensory ataxia due to polyneuropathy, alongside higher cognitive function disorders are one of the commonest causes of impaired walking.
Peripheral neuropathy: long term usually. effects balance due to lack of sensation, may be associated with pain or ulcers.
Proprioception
Feet: long term usually! Need for OPD podiatry and chiropody – one solution is training staff to cut nails to resolve immediate impact on pain and stability.
Few foot causes will require admission but pro-active management will reduce risk of falling.
Zoom out
Wider issues surrounding that person e.g. environmental e.g. home, social support, psychological support, including loneliness.
Injury vs confidence preventing walking – importance of pain control for injuries and access to supportive rehabilitation
Medications review will often find contributing medications e.g. sedation, postural stability, continence.
Long Term High Risk
Long term high risk: management strategies (including that RH doesn’t take away falls risk). high low bed/ sensors/ POC/ pendant again patient choice and capacity
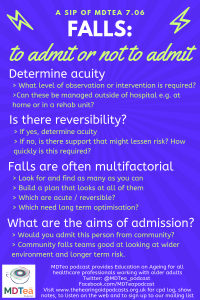
To admit or not to admit?
How to risk stratify for admission: needs acute hospital admission for the thing that is wrong rather than the fall itself.
Ask yourself:
- What is causing the fall – does the medical management need to be as an inpatient? Falls is not a diagnosis – admit for reason for fall if appropriate
- What needs to be in place at home for this person to have an acceptable level of risk vs safety.
- Are there short term goals for optimisation that could be helped by rehabilitation? multiple things that can be optimised together might indicate rehabilitation potential. Night time needs is a key consideration for bedded rehabilitation
- What does the person want? Shared decision making and autonomy
- Would I send this person to hospital for this vs should I admit? Cognitive bias of where seen: OPD vs ED, community teams often more comfortable with managing risk than hospital based teams
What interventions are people being admitted for?
- medical: monitoring / investigation / management only available in hospital
- nursing: care needs unable to be met at home e.g. wound care, delirious, medication administration, supervision of mobility
- physiotherapy + OT: functional ability requires aids not available elsewhere / intensity of therapy unavailable elsewhere, rehabilitation and assessment
Community services available influences decision
- rapid response teams
- voluntary sector e.g. red cross
- times of day available
- intensity of review required
Curriculum Mapping
This episode covers the following areas (n.b not all areas are covered in detail in this single episode):
- NHS Knowledge Skills Framework
- HWB3 Protection of health and wellbeing – Level 2
- HWB6 Assessment and treatment planning – Level 3
- HWB7 Interventions and treatments – Level 2
- G2 Development and innovation – Level 2
- G7 Capacity and capability – Level 2
- Foundation Curriculum (2016)
- 7. Works effectively as a team member – Interaction with colleagues
- 9. Recognises, assesses and initiates management of the acutely ill patient
- 10. Recognises, assesses and manages patients with long term conditions
- 11. Obtains history, performs clinical examination, formulates differential diagnosis and management plan
- Core Medical Training
- Blackout / Collapse
- Falls
- Geriatric Medicine
- GPVTS
- 3.05 Care of Older Adults
- HST Geriatric Medicine
- 3.1 Principal Learning Objectives – Section 8
- 3.2.2 Common Geriatric Problems
- 35 Falls
- 46 Falls and Syncope
- PA Matrix of conditions
- n/a
Feedback
We will add feedback to this as we receive it! The website will have the most up to date version always available: www.thehearingaidpodcasts.org.uk/mdtea





1 Response
[…] S7E6 – Falls: to admit or not? […]