10.4 Osteoarthritis
Presented by: Iain Wilkinson, Jo Preston, Sophie Norman
Special Guests: Helen Linklater, Tracy Szekely
Broadcast date: 27/04/2021
Supplementary interview
Social Media
Learning Outcomes
Knowledge
- To gain understanding of what OA is, and the pathophysiology underpinning it.
- To know when and how to investigate suspected OA
Skills
- To be able to explain OA to a patient
- To be able to manage OA
Attitudes
- To acknowledge the importance and existence of both pharmacological and non pharmacological management strategies in OA
- To acknowledge the impact living with OA has on patients and their day-to-day lives.
CPD Log
Show Notes
Definitions
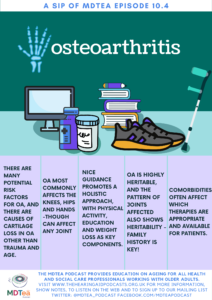
Osteoarthritis (OA) is a long-term chronic disease characterized by the deterioration of cartilage in joints which results in bones rubbing together and creating stiffness, pain, and impaired movement.
World Health Organisation 6.12 Osteoarthritis
Main discussion
Osteoarthritis (OA)…
- Is the most common form of arthritis.
- It affects all the tissues of the joint – cartilage, bone, ligaments, and muscles
- It can develop in any number of joints, but most commonly affects
- knees
- Hands
- Hips
- Cervical and lumbar spine
- Typically occurs later in life, usually after age 50,
- May start earlier in the case of joint injury
- When severe, OA is a painful condition that
- restricts mobility
- interrupts sleep
- interferes with the sufferer’s enjoyment of life
Osteoarthritis research society international
For the normal architecture of a joint, check out
https://www.versusarthritis.org/media/1266/what-is-arthritis-information-booklet.pdf
A joint with osteoarthritis will have, to varying degrees….
- Damage to the joint’s cartilage as it becomes less elastic and more brittle
- Bony spurs growing around the edge of the joint
- Swelling of the joint due to inflammation
- Inadequate lubricating synovial fluid for the cartilage and joint bones
- Breakdown of ligaments (tough bands that hold the joint together) and tendons (cords attaching muscles to bones)”
https://oarsi.org/patients
Pathophysiology of OA
One of the key concepts in OA is that there are other causes of cartilage loss besides age and trauma:
- Chondrocyte dysfunction and proliferation leads to changes in the extracellular matrix and metalloproteinase (eg MMP13) enzyme release, which contribute to cartilage damage.
- Proteoglycan degradation leads to oedema and micro-fissures in the cartilage, which can progress to causing damage to the underlying bone – in the form of cysts and erosions.
- Cartilage degradation products stimulate synovial inflammation and the production of pro-inflammatory cytokines e.g. IL-1 and TNF alpha.
This all points to an inflammatory component in osteoarthritis, with the presence of synovitis (membrane inflammation) +/- joint effusion (swelling) in almost half of patients. Macrophages predominate in this environment (part of the innate immune response), and this is different to what we see in inflammatory arthritis.
Macrophages in fatty tissue are a source of proinflammatory cytokines, and OA is associated with obesity. Obesity may be associated with a low level systemic proinflammatory state, and this is seen in inflammatory arthritis.
Not everyone with OA develops severe disease, and OA does not progress at the same rate in all patients.
Oxford Handbook of Rheumatology 2018
Several subsets of OA exist, including:
- Primary OA
- Generalised nodal OA – often MCP involvement, and then consider investigation for secondary causes
- Inflammatory/erosive OA – especially PIP joint involvement
- Large joint OA (knee and hip)
- Spinal OA
- Secondary OA
Primary causes
Risk factors associated with OA include the following:
- Genetic risk
- Increased concordance for OA in monozygotic (identical) vs dizygotic twins, and particularly for nodal OA
- Genome wide association studies have identified genetic loci associated with OA, different for hand (chromosomes 1,7,9,13,19)/knee (chromosome 13/hip (chromosome 11)
- Genetics of bone or articular cartilage structure
- Underlying metabolic conditions – eg calcium crystal deposition disease and acromegaly
- Obesity (close association with onset and progression of knee and hand OA, but not hip OA)
- Abnormal joints – eg femoral dysplasia (hip OA)
- Trauma (repeated or single event)
- Low vitamin D levels
Factors with less, or no, evidence for being a risk factor for OA:
- For hip OA: prior hip disease (e.g. Perthe’s disease), acetabular dysplasia, avascular necrosis of the femoral head, severe trauma, generalised OA, and occupation e.g. farming
- There is little evidence to link OA with repetitive injury from occupation or sports, such as running in those with normal joints, except perhaps knee-bending in men
https://pubmed.ncbi.nlm.nih.gov/11083262/
Secondary causes
- Trauma
- Metabolic/endocrine – haemochromatosis, acromegaly, hyperparathyroidism, ochronosis (alkaptonuria), Gaucher’s disease, hypothyroidism, Paget’s disease, osteonecrosis, haemoglobinopathy
- Secondary to inflammatory arthritis or infection
- Crystal deposition disease: calcium pyrophosphate, uric acid, hydroxyapatite
- Neuropathic disorders, e.g. Diabetes mellitus, syphilis, (Charcot joint)
- Anatomical abnormalities: bone dysplasia, biomechanical factors such as leg length discrepancy, varus/valgus deformity, scoliosis, joint hypermobility
Oxford Handbook of Rheumatology 2018
Rheumatology Secrets 2010
Investigation of OA
- This is based on clinical and radiological symptoms, and there are no specific diagnostic lab tests for primary OA
- Radiographs correlate poorly with symptoms and clinical function
- MRI is better at identifying cartilage loss, subchondral bone oedema, microfractures and synovitis, but is rarely used
Current management strategies
2019 OARSI guidelines for non surgical management of knee, hip and polyarticular OA
The OARSI guidelines advocate for and recommend
- Arthritis education
- Structured land-based exercise programmes
- Topical NSAIDs for knee OA
- Intra – articular corticosteroids
- Intra – articular hyaluronate
- Aquatic exercise
- They advise against paracetamol and advise strongly against opioids
- They acknowledgement the impact of comorbidity on available treatment options which is what we all encounter in clinical practice.
- No mention of systemic steroids which can offer benefit in OA
NICE guidance for osteoarthritis, updated Dec 2020
One of the overarching themes is the holistic and integrated approach.;
1 Recommendations | Osteoarthritis: care and management | Guidance | NICE
The guidance states that we should offer advice on the following;
- Access to appropriate information
- Activity and exercise
- Interventions to achieve weight loss
Activity and exercise advice should be offered IRRESPECTIVE of age, comorbidity, pain severity or disability, and should include
- Local muscle strengthening AND general aerobic fitness
- Manipulation and stretching should be considered as an adjunct
An NIHR review of exercise interventions in OA from 2018 looked at several outcome measures after exercise interventions, and found;
- Exercise reduced pain by 6%
- No change in functional ability was noted after exercise
- There was a slight increase in patients’ belief in their own abilities/capacity. a slight reduction in depression, but no effect on anxiety with exercise intervention
- Social function improved with exercise intervention.
Interviews of participants in the study revealed
- pain, other comorbidities, tiredness and own views of physical fitness levels impacted what type/amount of activity people felt able to do
- There was a belief amongst participants that pain meant joint damage.
- Clear instructions and advice on what would be experienced during exercise reassured participants.
How can we deliver this?
- 1:1 NHS physiotherapy referral
- Patient information and education with written/accessible material
- Charities eg versus arthritis have resources and support networks
- Group, individual and online programmes,
In response to COVID, Keele university and The Joint Effort Initiative Implementation group collated international OA management programmes to produce a repository of online, evidence based resources (endorsed by OARSI) for patients/training HCPs, based on NICE and OARSI guidelines including at least two recommended non pharmacological and non surgical interventions for OA (eg nutrition/weight loss, physical activity)
https://www.csp.org.uk/system/files/documents/2020-12/mike_hurleys_poster.p
ESCAPE-pain is one that is included – an integrated rehabilitation programme of education and exercise for OA
(ESCAPE-pain = Enabling Self-management and Coping with Arthritic Pain using Exercise)
NICE QIPP report on Escape-pain concluded that the programme;
- Is safe
- produces better clinical outcomes compared with management in primary care (Hurley et al. 2007a)
- Is as clinically effective and more cost effective than normal individual outpatient physiotherapy (Jessep et al. 2009).
Part of the programme discusses moving from considering OA in terms of biomedical model to that of biopsychosocial model
- In the biomedical model of osteoarthritis, correcting any abnormalities will require removal of the impairment and relieve the pain (irrespective of the wider psychological and social aspect of a person’s life).
Instead of seeing OA as a cycle of pathology that impairs normal function and leads to pain and disability as a consequence, the biopsychosocial model considers
- Health beliefs
- Social networks
- External environment
This addresses unhelpful health beliefs and behaviours (such as fear avoidance and catastrophizing), emphasises the importance of giving information and advice, and promotes self-management and coping skills.
The role of occupational therapists in OA;
An OT reviews work/household/leisure activities, and recommends interventions to facilitate/improve function in these areas.
They may suggest the following to patients with OA:
- using your hands differently
- positioning yourself more comfortably
- taking more rest breaks
- getting help with heavier jobs.
There’s a huge range of aids and appliances available e.g. chunky-grip pens, vegetable peelers, kettle-tippers, bath seats, raised toilet seats and stairlifts.
An OT might suggest vehicle adaptations to help patients with OA, such as a panoramic-view mirror if turning the head is difficult.
Online and social medial resources
- Infographic on OA as a Serious Disease
- https://twitter.com/heyOApodcast
- Chartered society for physiotherapy website – regional exercise resources
- @movingmedicine – supporting physical activity advice across England, collaboration with Faculty of Sports and Exercise Medicine UK, Public Health England UK and Sport England
- Versus arthritis – Arthritis care + arthritis research UK
- Videos – Let’s move with Leon
- Resources
- for coping with emotional and mental impact of OA, and during COVID
- Signpost to their online community to interact with others
- Helpline (not overnight)
- AI tool to direct users to arthritis relevant info in time of COVID
- Policy updates
- Research updates
Curriculum Mapping
Foundation Programme
- Clinically effective prescription
- Clinical management
- Support for patients with long term conditions
- Interaction with colleagues
GPVTS
- Musculoskeletal Health (clinical topic)
- Osteoarthritis including joint replacement surgery risks and complications
Internal Medicine Stage 1
- Rheumatology
- Osteoarthritis
Geriatric Medicine Specialty Training
- Poor mobility
- Osteoarthrosis
- Diagnosis and management of chronic disease and disability in older patients




