Episode 3.08: Peri-operative care
Presented by:
Dr Iain Wilkinson (Consultant Geriatrician East Surrey Hospital)
Dr Jo Preston (Consultant Geriatrician St George’s Hospital)
Broadcast date: 23rd May 2017
Click here for a PDF version of this infographic
We will be talking about …. The perioperative management of older people undergoing surgery… which is also the topic of a five part spin off series with associated e-learning course later this year – so if this whets your appetite then subscribe to the mailing list using the link in the top right hand corner of the website as we will send you details when it all goes live.
CPD log
Click here to log your CPD online and receive a copy by email.
Episode 3.08 Show Notes Peri-operative Care
Click here for a PDF version of these notes
Learning Outcomes
Knowledge:
- Multidisciplinary management of older patients perioperatively improves outcome
- Delirium is common post-operative complication in older people (especially cognitive impairment) and is associated with poor outcome
- Understand the basic principles of perioperative care
- To know that there are strategies for reducing perioperative risk
Skills:
- To be able to manage pain in an older patient
- To be able to identify patients at risk of delirium
- To be able to perform a perioperative risk assessment of an older person (NHFS/P-Possum/DEAR score)
Attitudes:
- Appreciate that proactive management of the older patient can improve outcome
- To appreciate the importance of a structured assessment
Social Media Spots this week
Ten tips for Redesign (via @semaj187 at an IHI summit on twitter), favourites including
- 85/85 rule: planning for what happens 85% of the time for 85% of events.
- Create methods to identify exceptions to the 85/85 rule so appropriate adjustments can occur.
- Always design 2nd and 3rd level plans for exceptions, rather than overdesigning for all events.
Post-anaesthetic dementia care project found on Academy of Fabulous NHS stuff website
- Dementia resource trolley: CD player, CDs, headphones, stress toys, twiddle muffs
- This is Me documents completed pre-operatively and available in recovery.
- Flexible learning for teams using podcasts
Definitions:
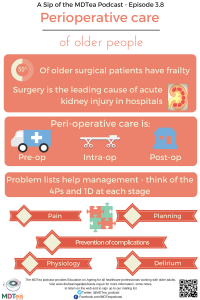
Peri-operative literally means around the time of surgery – no clear definition of time scales post-operatively really.
Practical Definition:
From a practical point of view, peri-operative covers the Pre-operative, intra-operative and immediate post-operative time… so really does involve the whole team from the front door to rehabilitation.
Review of literature
Over the last 20 years, the number of older people undergoing surgical procedures has increased faster than the rate of population ageing.
- Changes in anaesthetic and surgical techniques, patient expectations and increasing evidence of improved morbidity and mortality following surgery even in the oldest old
- However adverse postoperative outcomes, particularly medical complications still remain commoner in older > younger.
- Between 4.1 and 50.3% of all surgical patients have frailty. This wide variation relates to the issues of definition, measurement and varying populations studied (go back to season 2.1).
- Older patients are more likely to be frail (around 50%) – much greater than the background level in older people (around 10%).
A survey of 157 surgical trainees in the UK showed
- Trainees believe that they receive inadequate training in the perioperative management of complex, older surgical patients
- They are inadequately supported by geriatric medicine physicians.
- Trainee knowledge of geriatric issues such as delirium and mental capacity was poor.
- Surgical trainees support the concept of closer liaison and shared care of complex, older patients with geriatric medicine physicians.
We talked through a case to then illustrate principles of an approach. An 84 year old man with moderate COPD, CKD (stage 3), HTN, DM (not taking insulin) and with AF – on anticoagulation falls and sustains a hip fracture. He is usually independent at home in a house and walks with a stick.
Use a problem list to identify the key issues – work through these one by one (bottom up or top down).
At each stage think of 4 P’s and a D at each stage
- Pre op – Pain, Physiology and Planning and Prevention (of op) and Delirium,
- Intraoperative – Pain, Physiology and Planning (of recovery) and Prevention of complications and Delirium
- Post-operative – Pain, Physiology and Planning and Prevention of recurrence ( and Discharge)
The AABGI (Association of Anaesthetist of Great Britain and Ireland) state that:
The aims of peri-operative care are to treat elderly patients in a timely, dignified manner, and to optimise rehabilitation by avoiding postoperative complications. Effective peri-operative care improves the likelihood of very elderly surgical patients returning to their same pre-morbid place of residence, and maintains the continuity of their community care when in hospital.
Multidisciplinary care improves outcomes for elderly surgical patients. Protocol-driven integrated pathways guide care effectively, but must be individualised to suit each patient. The AAGBI strongly supports an expanded role for senior geriatricians in coordinating peri-operative care for the elderly, with input from senior anaesthetists (consultants/associate specialists) and surgeons.
Pre-operatively with our patient:
- Pain
- aiming to relieve pain asap from #.
- Opioid sparing if possible (may reduce delirium) – but above all something effective#
- Physiology
- Think about the problem list: Blood pressure in context of hypertension – not too high, not too low
- Diabetes – what is the blood glucose now? Think about what to do with this: IV insulin if on insulin otherwise probably just give their normal treatment.
- Heart rate? What is it? Do we need to worry about the heart? – ECG
- Renal function – important to try to protect this
- Surgery is a leading cause of AKI in hospitalized patients (the incidence ranges from 18% to 47% depending on the definition used).
- Risk Factors are: age, hypertension, diabetes mellitus, cardiac failure, peripheral vascular disease, cerebrovascular disease and chronic kidney disease (the most important probably).
- Prevention: Hydration, remove nephrotoxics prophylactically, maintain BP and avoid excess anaemia.
- Treat anaemia early!
- Prevention of complications
- Look for early signs of LRTI
- VTE prophylaxis
- Avoid hypoglycaemia
- Pain relief post op – needs to be sufficient to get up as soon as allowed.
- Planning
- Need to reverse Warfarin or other anticoagulants – follow your local protocols
- If you can wait for antiplatelet action to wear off – in reality only possible in low risk elective surgery
- Think about post op continence plan
- Post op plan for mobility
- Start thinking about d.c planning – early OT/PT input for background etc.
- Risk assessment – NHFS? ASA? – Delirium risk: http://www.riskprediction.org.uk/index-nhfs.php – numerous scores on this website.
- CPR / ceilings of care
Calvert, Shaw. (2012) Perioperative acute kidney injury Perioper Med (Lond).; 1: 6.
Intraoperatively – in theatre and the anaesthetic room…
- Pain – as pre op really – try to avoid over sedation – some suggestions this may help delirium
- Physiology
- Think about the anaesthetic agent and method of delivery (spinal or local vs general anaesthetic).
- Keep normothermia is at all possible
- Maintain BP stable (high risk times especially (post induction, or cement insertion).)
- Monitor blood loss during the operation and Hb soon post op
- Prevention of complications
- If you get it right – there are less complications!
- Planning
- Where are we going post op – HDU? Ward? Etc.
- When is the patient going to get out of bed?
- Anything to inform the ward team of (ie. large BP drop etc).
Post op: now back on the ward post procedure…
- Pain
- Same rules apply!
- Measure it regularly and do something about it early. Use visual scores such as the Abbey for people with dementia.
- Physiology
- Is there delirium?
- Postoperative delirium is common, but underdiagnosed, in elderly surgical patients, and delays rehabilitation. Multimodal intervention strategies are recommended for preventing postoperative delirium.
- Anaemia? – IV iron vs blood
- Blood sugar – back onto normal treatment post op
- Anti-hypertensives – gradually introduce usual medications – but use this time as an opportunity to review the need for treatment.
- Is there delirium?
- Prevention of complications
- Treat any infection early – especially in patients with reduced mobility
- Wound – look at it enough – but not too much!
- Mobilise out of bed early – how best to achieve these transfers – how often?
- Good mouth care
- Attention to mood and anxiety
- Discharge planning
- Goal directed rehabilitation – is further rehab needed / suitable etc.
- Regular MDT discussions with patient and team. – including the Social workers, who may or may not always be integral in the same way to the MDT – to assist with planning new/increased care needs/reinstating care.
However despite all these things:
The evidence base informing peri-operative care for the elderly remains poor. Anaesthetists are strongly encouraged to become involved in national audit projects and outcomes research specifically involving elderly surgical patients.
Curriculum Mapping:
This episode covers the following areas (n.b not all areas are covered in detail in this single episode):
| Curriculum | Area | |
| ~ Core Surgical Training |
Section
– Dementia – Peri-operative care |
|
| Foundation curriculum
(2016) |
Section
1.2 1.4 4.19 |
Title
Delivers patient centred care and maintains trust Keeps practice up to date through learning and teaching Makes patient safety a priority in clinical practice |
| Core Medical Training | Geriatric Medicine
Acute confusion / Delirium |
|
| GPVTS program | Section 2.03 The GP in the Wider Professional Environment
Section 3.05 – Managing older adults
|
|






1 Response
[…] S3E8 – Perioperative Care of Older People […]