Episode 1.9 Dizziness and Balance
MDTea Episode 9: Dizziness & Balance
Posted 10th May 2016
Presented by: Jo Preston (Consultant Geriatrician at St George’s Hospital) and Iain Wilkinson (Consultant Geriatrician at East Surrey Hospital).
Core Faculty: Adam Buckler – Pharmacist, Tracey Szekely – Occupational Therapist.
Guest Faculty: Gaggandeep Alg – Geriatrics Registrar
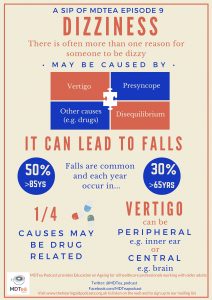
In this episode will look at the complex interplay of dizziness and balance and explore some of the causes of and importance of managing ‘dizziness’ in older people.
Click here for the show notes for this episode.
Here is a Sip of MDTea for this episode.
CPD log
Click here to log your CPD online and receive a copy by email.
Episode 9 Show Notes
Dizziness (and balance)
___
Presented by: Dr Jo Preston & Dr Iain Wilkinson
Faculty:
Tracey Szekely, Adam Buckler, Dr Gaggendeep Alg
Broadcast Date: 10th May 2016
Learning Outcomes
Knowledge:
- To understand the physiological mechanisms that contribute to balance, and how these can go wrong in older people
- To know the common causes of balance disorders in older people
Skills:
- To be able to identify potential causes for the symptom of ‘dizziness’ and use alternative words to describe this
Attitudes:
- Understand that balance disorders may have a large effect on the quality of life of an older adults
Definitions:
Formal / Scientific Definition:
Dizziness: a term used to describe a range of sensations, such as feeling faint, woozy, weak or unsteady. Dizziness that creates the false sense that you or your surroundings are spinning or moving is called vertigo.
Postural stability / balance can be defined as the ability of an individual to maintain the position of the body (more specifically, its centre of mass) within specific boundaries of space. Maintaining postural stability requires the complex integration of many sensory inputs (ear, eyes, brain and joints) which is then processed by the brain and actions are carried out to keep us upright.
Practical Definition:
Practically dizziness is intertwined with balance and postural stability. When you feel dizzy there is a mismatch between the inner ear or vestibular system and the visual system and the somatosensory system. A clear description of the symptoms is really important and takes time to unpick exactly what the patient means when they say they are ‘dizzy’.
Key Points from Discussion
Try to get detail in the history from your patients – what do they mean when they say they feel dizzy? What were they doing at the time? What other symptoms did they have?
Symptom complexes
Pre-syncope – That feeling just before you faint. May well need further investigation, and refer to the transient loss of consciousness guidelines as to how to do this.
European Society of Cardiology Guidelines (2009)
Vertigo
Related to vestibular function – can be peripheral or central.
The head impulse test can help with working out one from the other.
Videos on Imperial website also
Vestibular reflexes and positional manoeuvres
| Characteristic | Peripheral (are the most common eg. VN / BPPV) | Central |
| Starting | Sudden | Insidious |
| Clinical Picture | Paroxysmal | Continuous |
| Intensity | Maximum = initial | Mild |
| Duration | Minutes / hours | Days / Weeks |
| Vertical Nystagmus | Absent | Common |
| Influence of Movement | Marked | Mild or none |
| Tinnitus / Deafness | Common | Absent |
Disequilibrium
Really a problem with gait and walking – can be lower level, mid level or higher level.
Lower level is problems with the sensory inputs – outside of central nervous sytem – eg. peuph. neuropathy / musculoskeletal problems or vision.
Middle – a central problem – e.g Basal ganglia – PD, Cerebellum – Ataxia, hemiplegic. There is a link between the structure and the problem.
Higher – Problem with the higher cognitive function – eg. cautious gait (e.g fear of falling in episode 5)
Treatments:
Specific manouvers and vestibular rehabilitation
Mini GEM video on balance assessment – on youtube by AEME
Other – non-specific
- Medications can be a large cause for patients ‘dizziness’ symptoms and the article below explores this in more details. Adjusting the medications may be a quick win with some patients to remove a proportion of their symptoms.
Causes of persistent dizziness in elderly patients in primary care
Curriculum Mapping:
This episode covers the following areas (n.b not all areas are covered in detail in this single episode):
| Curriculum | Area |
| NHS Knowledge Skills Framework | Suitable to support staff at the following levels:
|
| Foundation Curriculum 2012 | 1.3 Continuity of care
1.4 Team working 2.1 Patient as centre of care 7.9 Interface with different specialities and other professions |
| Foundation Curriculum 2016 | 2. Patient cetred care
4. Self-directed learning 6. Interface with other healthcare professionals 11. Diagnosis |
| Core Medical Training | Common competences:
Symptom based competences:
System specific competences:
|
| GPVTS program | Section 2.03 The GP in the Wider Professional Environment
Section 3.05 – Managing older adults
Section 3.15 – Care of people with ENT, Oral and Facial problems
|
| ANP (Draws from KSF) | 7.11 Syncope, pre-syncope, dizziness
7.20 Falls, dizziness, syncope 13. Therapeutics and safe prescribing |
| Physician Associate – Core clinical conditions | Section 7.1.5 – Vertigo |




