Episode 3.02 – Constipation
Presented by:
Dr Iain Wilkinson (Consultant Geriatrician East Surrey Hospital)
Dr Jo Preston (Consultant Geriatrician St George’s Hospital)
Mairead O’Malley (Specialty Pharmacist, Brighton and Sussex University Hospitals)
Faculty:
Clare Watson (Nurse, Brighton and Sussex University Hospitals)
Wendy Grosvenor (Dementia Nurse Specialist and Lecturer at University of Surrey)
Guest faculty:
Dr Gaggandeep Singh Alg (Geriatric and General Medicine Registrar, Royal Berkshire Hospital)
Broadcast date: 28th February 2017
Click here to download a printable PDF version of the infographic
CPD log
Click here to log your CPD online and receive a copy by email.
Episode 3.02 Constipation – Show Notes
Click here for a downloadable PDF version of the Show Notes
Learning Outcomes
Knowledge:
- To understand the causes of constipation in older people
- To understand the principles of constipation treatment in older people
- To develop an understanding of the normal gut physiology in older people
Skills:
- To be able to take a bowel frequency history from a patient
- To be able to recommend non-pharmacological measures to people with constipation
Attitudes:
- To understand that clinician and patient may have different definitions of constipation
- To understand the potential impact of chronic constipation on a older person’s life.
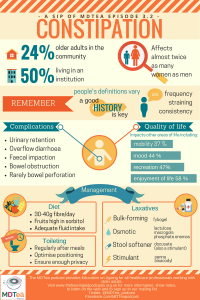
Definitions: Constipation is not a disease entity in itself. Clinical and research literature documents that patients and clinicians use different definitions of constipation:
- Frequency
- Passing stool less than once every 3 days.
- Consistency
- Hard stool.
- Difficulty
- Initiating evacuation despite regular bowel motions.
- Feeling of incomplete evacuation.
Practical Definition: It’s really quite subjective. A study of 531 general practice patients found that 50% of them gave a different definition of constipation than their physicians
Constipation: a different entity for patients and doctors Fam Pract. 1996 Apr;13(2):156-9.
Key Points from Discussion
Because of the subjective nature of the definition it is important to establish patient’s normal frequency:
- Some patients have a bowel motion once a week and that is their normal and others 2/3 times per day.
- Think if they have a stoma, what’s normal for them – may need medical review etc. Constipation in context of a stoma could be more serious.
Either way it is much more common in older patients.
- 10-15% of adults in developed countries.
- Twice as frequently in women as in men (see the pelvic floor comments below)
- Highly prevalent in the elderly,
- 50% of those living in an institution
- A survey of community-‐dwelling elderly (65-‐93 years old) found a prevalence of chronic constipation of 24%.
Prevalence of gastrointestinal symptoms in the elderly: a population based study
MAKING THE DIAGNOSIS
To diagnose constipation you are relying on the patient to self-report that defecation is unsatisfactory or for a HCP to identify this.
- Care homes likely to be familiar with their residents normal bowel care plan – in hospital staff will not have this familiarity therefore reliance on stool charting is required.
- We usually use the Bristol stool chart to assess stool type – this is really important for inpatients too. NB when bowels haven’t opened this needs recording too!!
Patients may also describe feelings of incomplete evacuation, irritability, lack of appetite and malaise. A detailed history is needed.
- Some data suggest that older adults perceive constipation as straining during defecation rather than decreased bowel frequency.
- Another study of elderly individuals who reported constipation demonstrated that straining and hard bowel movements were the most frequent complaints.
- Embarrassment factor… a patient may not have raised this before, or are other things more important to them
Prevalence of gastrointestinal symptoms in the elderly: a population-based study
A determination of the most likely aetiology for constipation requires identification of the primary complaint
- Stool hardness (may point to dehydration etc.)
- Problems with the act of defecation (may point to muscular or neurological etc.)
There are a long list of medications that can cause constipation, including:
- Medications which affect transit time, for example pain killers opiates/codeine, antispasmodics, aluminium containing antacids, anticholinergics, verapamil
- Medications that cause water loss or reduced transit, for example diuretics, antihypertensives
IMPACT OF CONSTIPATION Complications
- Urinary Retention
- Overflow Diarrhoea
- Bowel Obstruciton
- Rarely Bowel Perforation
- Faecal impaction
Quality of life
- In the most severely affected individuals, chronic constipation is accompanied by very marked impairment in quality of life and social functioning.
- Chronic constipation-associated GI symptoms significantly interfere with many aspects of sufferers’ daily lives, including:
- mood (44%),
- mobility (37%),
- normal work (42%),
- recreation (47%), and
- enjoyment of life (58%)
- The impact of chronic constipation on quality of life for patients is comparable with that for conditions such as COPD, diabetes and depression.
COMPASS Therapeutic Notes on the Management of Chronic Contipation in Primary Care 2016
Cost In Northern Ireland in the 12 months to June 2016 almost 700,000 prescriptions were filled for laxatives and newer agents for constipation, at a cost of nearly £4million
TREATMENT
1. Non-pharmacological
- Increase dietary fibre. Decrease in portion sizes and lack of dietary fibre lead to reduced motility (Toner and Claros 2012). 18g per day of fibre recommended by the British Nutrition Foundation – UK average round 12g. One Study showed that we should be aiming for 30-‐40g of fibre per day.
Schiller L, The therapy of constipation
- Sorbitol is a naturally occurring sugar. It is not digested very well and draws water into the gut, which has an effect of softening the stools. In effect, it acts like a natural osmotic laxative. Fruits (and their juices) that have a high sorbitol content include apples, apricots, gooseberries, grapes (and raisins), peaches, pears, plums, prunes, raspberries and strawberries. The concentration of sorbitol is about 5-10 times higher in dried fruit.
- Ensure adequate fluid intake to maintain both bowel contents and normal transit time
- Maintain mobility – immobility can reduce muscle tone in the bowel and abdominal walls leading to constipation
Holman et al 2008, Costilla and Foxx-Orenstein 2014
- Review toileting conditions, such as:
- Lack of privacy
- Waiting for busy staff
- Position- especially knee position- see Squatty Potty
- Regular toileting – making use of the Gastrocolic reflex
- Think about timing of care visits and reassess if needed
2. Pharmacological
- Bulk forming laxatives e.g. Fybogel
Pharmacodynamics – Increase the bulk of stools by enabling fluid to be retained within the faeces. Increasing the mass increases peristalsis. Must have adequate fluid hydration to prevent intestinal obstruction. Caution with frail. Not suitable for those taking opioids.
- Osmotic laxatives – Lactulose/Macrogels/Phosphate enemas
Pharmacodynamics – soften the stool makes them easier to pass by increasing the amount of water in your bowels. Lactulose causes increased bloating and colic symptoms. Movicol / Laxido volume can be difficult for those to drink or those who are fluid restricted (125mls per sachet) typical dose would be 2-4 sachets. Movicol-half is available (60mls per sachet). Can affect medication absorption.
- Stimulant Bisacodyl/Senna
Pharmacodynamics – stimulating nerves that control the muscles lining the digestive tract. Senna – Short term license only. Stimulates muscle in the wall of the large bowel to squeeze harder than usual, pushing stools along and out. Their effect is usually within 8-12 hours. A bedtime dose is recommended so you are likely to feel the urge to go to the toilet sometime the following morning. Stimulant laxative suppositories act more quickly (within 20-60 minutes). They need to be against the rectal wall. Possible side-effects from stimulant laxatives include abdominal cramps, and long-term use can lead to a bowel that is less active on its own (‘lazy bowel’).
- Stool softener laxatives – Docusate (stimulant activity also)
Pharmacodynamics – ‘Surface wetting agent’. Does what it says on the tin. Makes the surface of the stools permeable, water can be absorbed, which increases the fluid content of hard stools.These work by wetting and softening the faeces. The most commonly used is docusate sodium (which also has a weak stimulant action too). Liquid paraffin used to be commonly used as a faecal softener. However, it is now not recommended, as it may cause side-effects, such as seeping from the anus and irritation of the skin, and it can interfere with the absorption of some vitamins from the gut. Glycerin Suppositories work mostly by hyperosmotic action, but the sodium stearate in the preparation also causes local irritation to the colon
COMPASS Therapeutic Notes on the Management of Chronic Contipation in Primary Care 2016
FUNCTIONAL BOWEL DISORDERS
Most constipation is ‘functional’ in nature – the rest likely to ‘pathological’ or ‘iatrogenic’ – caused by drugs.
- “Functional” is used to describe symptoms or problems that have no underlying anatomic abnormalities. However…the normal ‘function’ of an organ has changed. Functional bowel disorders, including functional constipation, are diagnosed primarily through patients’ reporting of symptoms.
- As a result, a symptom based classification is needed for clinical diagnosis, evidence based management, and research
- Since 1989, an international panel of experts has met four times and issued recommendations on the diagnosis and management of Irritable Bowel Syndrome (IBS), as well as diagnostic criteria for other functional bowel disorders. Known as the Rome I, Rome II, and Rome III criteria, these recommendations have evolved to include functional anorectal disorders.
Pathophysiology of constipation in the older adult
PHYSIOLOGY OF THE BOWEL
- Digestive tract is from the mouth to the anus with endocrine and metabolic systems inclusive.
- Normal stool output is about 200 mg daily.
- Activity in the proximal colon determines the consistency and volume of delivery of contents to the rectum. The rectum is a reservoir. As rectal filling gradually proceeds, anorectal sampling permits subconscious perception of the consistency of the content.
- An intact internal anal sphincter (IAS) ensures continence.
- Gastrointestinal motility
Gut transit time is not generally changed in elderly volunteers, but does seem to be exquisitely sensitive to thyroid hormone status and can be considerably prolonged even in subclinical hypothyroidism
- Age-related neurodegenerative changes in the enteric nervous system (ENS) may be key to functional changes observed with advanced age. In colons of people older than age 65, a 37% loss of enteric neurons was found when compared with younger people
- Rectum Mechanical changes (i.e. muscle) in the rectum probably cause most of the problems old people suffer in evacuating as well as the increasing prevalence of faecal incontinence with increasing age.
- A reduction in rectal wall elasticity means that tonic activity of the external sphincter is lost at a smaller volume.
- An age dependent increase in rectal pressure needed to produce an initial sensation of rectal filling has been found
- Maximum resting anal pressure and maximum squeeze pressure have been shown to decline with age, particularly in postmenopausal women.
Age related changes in gut physiology and nutritional status
Resources If you have some links or resources you’d like to share, get in touch and we’ll add them here. Twitter @MDTea_podcast Facebook www.facebook.com/MDTea or email thehearingaidpodcasts@gmail.com Curriculum Mapping: This episode covers the following areas (n.b not all areas are covered in detail in this single episode):
| Curriculum | Area |
| NHS Knowledge Skills Framework | Suitable to support staff at the following levels:
Personal and people development level 1-3 Service improvement level 1 |
| Foundation Curriculum 2012 | 2.1 Treats patient as centre of care
6.1 Lifelong learning 6.2 Evidence and guidelines 7.5 Safe prescribing 10.3 Nutrition 10.5 Health promotion, patient education and public health |
| Foundation Curriculum 2016 | 2. Patient centred care
4. Self-directed learning 6. Interface with other healthcare professionals 13. Prescribes safely – Guidance on prescription – Review of prescriptions 16. Demonstrates understanding of the principles of health promotion and illness prevention |
| Core Medical Training | Common competences:
Symptom based competences: Abdominal swelling and constipation System specific competences:
|
| GPVTS program | Section 3.05 – Care of older adults
Section 3.13 Digestive Health
|
| ANP (Draws from KSF) | Section 7.9 Constipation, diarrhoea, faecal impaction Section 13 Therapeutics and safe prescribing Section 19. Managing long term conditions and promoting patient self-care Section 20. The patient as central focus of care |
| PA Matrix of conditions | Conditions in Category 1A: 4.3.1 Constipation/faecal impaction |
Feedback We will add feedback to this as we receive it! The website will have the most up to date version always available: www.thehearingaidpodcasts.org.uk/mdtea Find Us! To listen to this episode head to our website, itunes or stitcher. Give us feedback by emailing us, via twitter or facebook. Check out our cool infographic A sip of… summarising 5 key points on topic. It’s made for sharing!




