Episode 2.07 – Foot Health
 In this episode we will be discussing all things foot and feet based!
In this episode we will be discussing all things foot and feet based!
Broadcast date is 15th November 2016.
Here is a sip of the MDTea to download…
Presented by: Jo Preston (Consultant Geriatrician at St George’s Hospital), Iain Wilkinson (Consultant Geriatrician at East Surrey Hospital) and Amy Heskett (Community Geriatrician in Kent).
Core Faculty: SJ Ryan (Physiotherapist and Lecturer at University of Brighton).
Guest Faculty: Simon Otter (Podiatrist and Lecturer at University of Brighton).
CPD log
Click here to log your CPD online and receive a copy by email.
Resources for Self Management
Fitter Feet from AgeUK
Personal Foot Care Guidance from NHS Scotland
Episode 2.07: Foot Health – Show Notes
Click here to download these.
Learning Outcomes
Knowledge
- To know the importance of good foot health and feet care in older adults
- To understand the impact of foot health on mobility and falls in older adults
Skills
- To be able to assess basic foot health and signpost the older person to further assessment
Attitudes
- To understand that feet are a core aspect of mobility and impact on a person’s quality of life
So what is foot health exactly?
Foot health can be split into 2 parts
-
- Form – skin quality, nails,
- Function – range of movement, joint articulation, support structures etc.
This is a big problem in older adults. One study from 1997 found 53% of patients >60yrs had more than 3 problems with their feet.
Foot morbidity and exposure to chiropody: population based study. Harvey et. al BMJ 1997 pubmed link
Function of the feet:
- Feet are complex structures!
- Each foot contains 26 bones and more than 100 ligaments
- The skin on the feet has more than 7,000 nerve endings
- In normal gait the foot is the only contact with the ground – so abnormalities or problems here logically lead to an increased risk of falls or gait problems.
- 176 pts in a retirement village underwent tests of foot and ankle characteristics (ROM etc) and other physiological falls risk factors (e.g vision, sensation)) and were followed for 12 months to determine the incidence of falls.
- Results. 41% reported falling during
- Fallers had: decreased ankle flexibility, more severe hallux valgus (literally toe out) deformity (Bunions), decreased plantar tactile sensitivity, and decreased toe plantarflexor strength; they were also more likely to have disabling foot pain.
- Discriminant function analysis revealed that decreased toe plantarflexor strength and disabling foot pain were significantly and independently associated with falls after accounting for physiological falls risk factors and age.
- Foot and ankle problems increase the risk of falls in older people. Interventions to address these factors may hold some promise as a falls prevention strategy.
- 176 pts in a retirement village underwent tests of foot and ankle characteristics (ROM etc) and other physiological falls risk factors (e.g vision, sensation)) and were followed for 12 months to determine the incidence of falls.
Foot and ankle risk factors for falls in older people: a prospective study. Menz et. al J Gerontol A Biol Sci Med Sci. 2006
Common foot problems include
- Foot pain – eg. Stiffness and arthritis
- Reduction in range of movement
- ‘Skin’ Problems – particularly important in diabetes / peripheral neuropathy:
- Toenail – including hardened or ingrown nails
- Toe deformities such as overlapping toes and bunions
- Skin problems – Corns, calluses, infections etc
- Footwear related – rubbing, blisters etc.
Good foot care therefore is important as it can lead onto:
- Reduced pain – painful feet can impair balance and functional ability;
- Increased mobility and physical activity – foot problems are a major causes of walking difficulties in older people;
- Increased self-esteem;
- Increased social contact and participation in leisure and cultural activities;
- Reduced risk of trips and falls – foot pain can cause people to wear loose footwear, which can contribute to falls.
Foot assessment and care for older people. Soliman & Brogan Nursing Times 2014. Link
- Poor foot care is a common problem for practical reasons (it’s hard to self manage) and affects many people. For example -Age Concern study):
- 31% of older people are unable to cut their own toenails because they:
- Can no longer reach their toenails;
- Are unable to handle nail clippers due to arthritis;
- Have conditions that make them feel dizzy if they bend;
- Have visual impairment;
- Have toenails that have become too thick to cut (Age Concern, 2007).
- 31% of older people are unable to cut their own toenails because they:
- Patients with diabetes: around 20% of people with DM will develop foot problems. These need specialist review by podiatrists if they develop any problems.
Primary Concerns, Older People’s Access to Primary Care by Age Concern (now AgeUK) 2007 : link
The DH (2009) describes foot care in two parts: that which someone can do themselves, and that which requires a trained professional.
1) What you can do yourself:
- Toenail cutting
- cutting and filing toenails safely, and keeping them at a length which feels comfortable.
- Skincare
- smoothing and moisturising dry and rough skin
- (Xerosis – dry skin – a common problem in older patients. 28 days of topical treatment… may however need much longer treatment as the protective barriers in the skin degrade with age and the skin is less resistant to damage from serous fluids. – the regularity of application is as important as the formulation)
- Moisturising cream should be applied every day, avoiding the area between the toes, which may become too moist and split;
- checking for cracks and breaks in the skin and signs of inflammation
- looking for signs of infection or other obvious early problems and referring for further professional advice.
- smoothing and moisturising dry and rough skin
2) That which needs a trained professional (nurse, Dr, Podiatrist, OT, PT etc).:
- Footwear advice
- reviewing footwear to assure safety and stability
- advising on suitability and how and where to obtain appropriate socks, shoes and other footwear. – senior rehab podcast
- encourage wearing of comfortable, well-fitting and supportive shoes rather than slippers
- Prevention advice
- keeping feet clean, dry, mobile, comfortable and warm
- promoting good foot health advice based on each individual’s lifestyle and circumstances.
- Signposting (direct re feet or opportunistic re. Falls / social care etc)
- recognising that foot conditions can change and, in the instance of pain, infection or other unreported conditions, knowing when to refer to podiatrists or other healthcare professionals (Ortho / orthotics etc)
- raising other health and social care risks with appropriate professionals including health and safety issues, social exclusion and benefit rights.
- Use foot care as part of a holistic assessment of patients and potentially part of forming a person centred treatment plan
- Problems with the feet may be the trigger for a wider assessment (e.g social care needs / medical optimisation)
Footcare services for older people: a resource pack for commissioners and service providers – DOH (2009): link
Recommendations for managing cutaneous disorders associated with advancing age. Humbert et al. Clin Interv Aging. 2016. Pubmed link
Foot pain also leads to a reduced quality of life. One study of 312 community-dwelling men and women age >60 years found that:
- Older people with disabling foot pain exhibit reduced HRQOL, functional impairment, and alterations to foot function that may contribute to an increased risk of falling.
- Providing interventions to older people to reduce foot pain and improve foot function may play a role in improving mobility and quality of life.
Similar findings in other similar studies looking hallux Valgus pain (Bunion) but there are no good studies to see the effect of addressing these though.
Cross-sectional analysis of foot function, functional ability, and health-related quality of life in older people with disabling foot pain. Mickle et al. Arthritis Care Res (Hoboken) 2011
The ideal shoe to minimise problems….
A review was conducted into this and found there are a large number of areas to be considered:
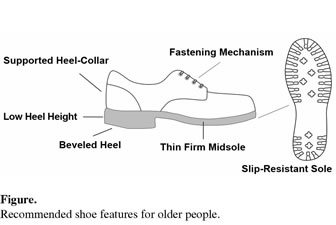 Shoes were better than being barefoot
Shoes were better than being barefoot- Low heel height versus high heels. High heels lead to lower walking speed, shorter step and increased cadence.
- Sole cushioning should be hard rather than soft. Thick- and soft-sole shoes impair stability during walking by reducing foot position awareness and mechanical stability, and may pose an even greater threat to stability during challenging task.
- Sole thickness should be thin for similar reasons
- Sole flaring – the jury is out… Wider soles in trainers which are less slippy but no evidence in older people
- Sole tread should be present on the sole and the heel.
One review of orthoses found that they can improve postural stability via a somatosensory or biomechanical effect. Using footwear with the proper features can be an appropriate intervention in order to increase the balance in the older population and reduce falls.
A systematic review of the effect of foot orthoses and shoe characteristics on balance in healthy older subjects. Aboutorabi et al. Prosthet Orthot Int. 2016
Curriculum Mapping
| Curriculum | Area |
| NHS Knowledge Skills Framework | Suitable to support staff at the following levels:
|
| Foundation Curriculum 2012 | 1.3 Continuity of care
1.4 Team working 2.1 Patient as centre of care 7.9 Interface with different specialities and other professions 10.1 Long-term conditions 10.5 Health promotion, patient education and public health |
| Foundation Curriculum 2016 | 2. Patient centred care
4. Self-directed learning 10. Management of long term conditions in the acutely unwell patient 10. Support for patients with long term conditions 16. Demonstrates understanding of the principles of health promotion and illness prevention |
| Core Medical Training | Common competences:
Symptom based competences:
System specific competences:
|
| GPVTS program | Section 2.03 The GP in the Wider Professional Environment
Section 3.05 – Managing older adults
Section 3.20 – Care of people with musculoskeletal problems |
| ANP (Draws from KSF) | Section 6. Clinical examination
Section 7.26 Immobility and declining mobility Section 10. CGA process |
| Physician Associate | Category 1A
5.6 Disorders of the Ankle/Foot |




