6.04 Ageing Lungs
In this episode we look at the ageing lungs, both what’s normal as we age and what’s abnormal. We will talk through some of the commenest conditions we see qffectinathe lungs in older people.
Presented by: Dr Jo Preston, Dr Iain Wilkinson with prior recording from Professor Allen.
Faculty: Sarah Jane Ryan – Physiotherapist University of Brighton
Social media this week
Iain:
Jo: Tweet from Dan Thomas:
Dementia research priorities chosen by people with dementia
I suspect the bulk of all dementia research budget is currently spent on immunotherapy targetting amyloid when the list below is what matters to people with dementia
From @AGSJournal pic.twitter.com/oTSjPBqR9E
— Dan Thomas (@dan26wales) August 14, 2018
The Gallery:
Learning outcomes
Knowledge:
To be able to describe and understand the normal changes in older people’s lungs.
To understand the impact of frailty on an older persons response to an respiratory insult
Skills:
To be able to describe spirometry to a patient
To be able to signpost people to ways to improve their inhaler technique
Attitudes:
To promote smoking cessation for all patients with lung disease
Show Notes
1. Introduction
This episode is based around an interview in did with professor Steven Allen back in 2013. As such we apologise for the sound quality being a bit less good than normal!
- ‘Dyspnoea’
- present in 32% of patients >70 yrs
- Poorer functional status
- Poorer physical and mental health
- More likely to be anxious and depressed
- Presence of LVF, airways disease and obesity were all higher in this group
- 60% of all presentations with dyspnoea are age >65yrs
- But… in older people it’s difficult to evaluate
- Subjective
- Small margin between disease and physical (FEV1 reduces with age)
- deconditioning (due to age or fitness levels)
- Gets more common as age increases
- Vary according to severity
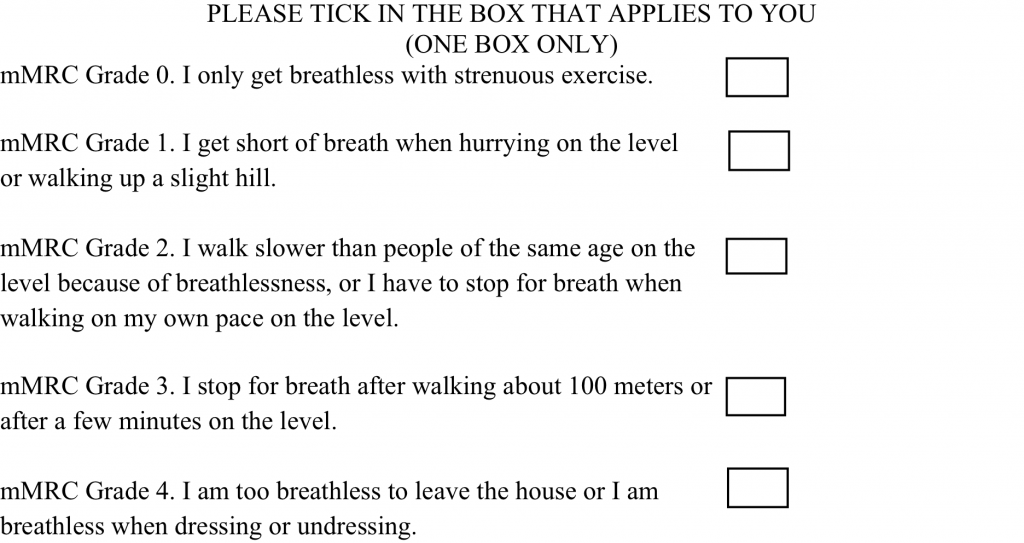
- MRC >2 = 36%, >3 = 16% >4 = 4%
- But… in older people it’s difficult to evaluate
- Cardiac and respiratory causes of SOB account for 70% of cases (others are neuro, anaemia etc)
COPD
Common:
- 5% of all global deaths are due to COPD
- Exposure to tobacco smoke is the main cause (some are due to long term asthma) [DON’’T talk about cessation – this comes later]
- 1.2 million ppl living with COPD in UK
- 4% ppl >40yrs old!
Main symptoms are:
Dyspnea: Progressive, persistent and characteristically worse with exercise.
Chronic cough: May be intermittent and may be unproductive.
Chronic sputum production: COPD patients commonly cough up sputum.
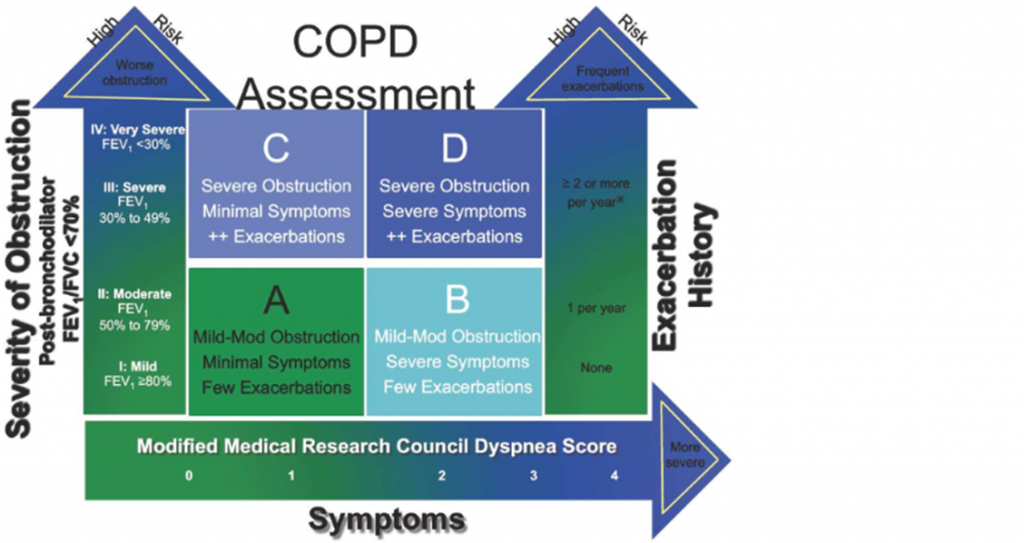
The goals of COPD assessment are to determine the severity of the disease, including the severity of airflow limitation, the impact on the patient’s health status, and the risk of future events.
COPD patients are at increased risk for:
- Cardiovascular diseases
- Osteoporosis
- Respiratory infections
- Anxiety and Depression
- Diabetes
- Lung cancer
- Bronchiectasis
Global Initiative for Chronic Obstructive Lung Disease
- The response to hypoxia or hypercapnia is markedly impaired in older adults (less respiratory reserve – frailty)
- A 50% reduction in response to hypoxia
- A 40% reduction in response to hypercarbia.
- Aging is associated with loss of potentially protective mechanisms in a population that is more likely to be exposed to these states, making them more vulnerable.
Asthma
“Central to all definitions is the presence of symptoms (more than one of wheeze, breathlessness, chest tightness, cough) and of variable airflow obstruction. More recent descriptions of asthma in both children and adults have included airway hyper-responsiveness and airway inflammation as components of the disease”
- The diagnosis of asthma is a clinical one.
- The absence of consistent gold-standard diagnostic criteria means that it is not possible to make unequivocal evidence-based recommendations on how to make a diagnosis of asthma.
- There is the possibility that there will be people at high probability of asthma in whom a ‘monitored initiation of treatment’ is appropriate without necessarily awaiting further investigation.
Patients with asthma often had the condition in their younger years.
Spirometry
- Spirometry is positioned as pivotal by both guidelines (BTS and NICE), but both caution that it is not useful for ruling out asthma because the sensitivity is low, especially in primary care populations (only 27% of people diagnosed as having asthma in the NICE feasibility work had obstructive spirometry which is similar to the estimate in BTS/SIGN of ‘a quarter having obstructive spirometry’).
“Spirometry is a method of assessing lung function by measuring the volume of air that the patient is able to expel from the lungs after a maximal inspiration. It is a reliable method of differentiating between obstructive airways disorders (e.g. COPD, asthma) and restrictive diseases (where the size of the lungs is reduced, e.g. fibrotic lung disease). Spirometry is the most effective way of determining the severity of COPD”
- There are spirometers in about 70–80% of practices in the UK and their use is increasing, particularly since changes to the GMS primary care contract introduced in April 2004.
- Practice nurses predominantly perform the tests but many lack confidence in carrying out the procedure or in the interpretation of the results.
- Accurate spirometry can only be performed with appropriate training.
- Most nurses and GPs request more help in carrying out and interpreting spirometry.
Spirometry in practice – A Practical Guide To Using Spirometry In Primary Care – BTC COPD Consortium
Smoking cessation
- Link to evidence of health care intervention here (in wellbeing episode I think we did this a bit)
- Death and ill health due to smoking-related diseases, particularly lung cancer, chronic obstructive pulmonary disease, and heart disease.
- Stopping smoking at age 60, 50, 40, or 30 adds about 3, 6, 9, or 10 years of life expectancy respectively [Doll et al, 2004].
- Less evidence in methods in the over 50s but all methods (pharmacological, non-pharmacological and multi-modal) worked significantly when compared with control groups.
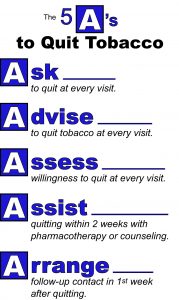
- There graphics are from the US clinical practice guideline for smoking cessation.
- In England — the free Smokefree National Helpline on 0300 123 1044 or online www.nhs.uk. This offers support via a smartphone app, email programme, text messages and Facebook page.
- In Scotland — the free Smokeline on 0800 84 84 84, or online www.nhsinform.scot.
- In Wales — the free Help Me Quit Wales Helpline on 0800 085 2219, or online www.helpmequit.wales.
- In Northern Ireland — online www.want2stop.info.
Inhaler useage
- Evidence suggests a negative correlation between advancing age and correct technique across MDI and varying DPI devices when examined collectively.
- Therefore think about who will be able to help them use the inhaler.
- Use spacers
- Less frequent medication delivery
https://www.asthma.org.uk/advice/inhalers-medicines-treatments/using-inhalers/
Curriculum Mapping
| Curriculum | Area |
| NHS Knowledge Skills Framework | Suitable to support staff at the following levels:
|
| Foundation curriculum | Section
10. Management of long term conditions in the acutely unwell patient 11. Obtains history, performs clinical examination, formulates differential diagnosis and management plan 13. Prescribes safely |
| Core Medical Training | Respiratory Medicine
Geriatric Medicine |
| HST Geriatric Medicine | 3.2.1 Basic Science and Biology of Ageing
3.2.3 Presentations of Other Illnesses in Older Persons – Respiratory 11. Managing Long-Term Conditions and Promoting Patient Self-care 29. Diagnosis and Management of Chronic Disease and Disability |
| GPVTS program | Section 2.03 The GP in the Wider Professional Environment
3.03 Care of Acutely Ill People – Asthma Section 3.05 – Managing older adults
3.19 Respiratory Health |
| PA matrix of conditions | Obstructive Pulmonary Disease
Infectious Respiratory Disorders |
| ANP (Draws from KSF) | Section 7.16 Chronic Obstructive Pulmonary Disease (COPD)
Managing Long-Term Conditions and Promoting Patient Self Care |