4.10 BPSD – Behavioural and Psychological Symptoms of Dementia
Episode 4.10 BPSD – Behavioral and Psychological Symptoms of Dementia
Presented by: Dr Jo Preston & Dr Iain Wilkinson
Faculty: Dr Victoria Osman-Hicks, Consultant Old Age Psychiatrist. Dr Cate Bailey, Old Age Psychiatry ST5 Trainee. Pam Tragmar, Physician Associate.
Broadcast Date: 19th December 2017
Sip of MDTea (pdf here)
Broadcast date: 7th November 2017
CPD log
Click here to log your CPD online and receive a copy by email.
Episode 4.10 Show Notes – Behavioral and Psychological Symptoms of Dementia (pdf here)
Learning Outcomes
Knowledge:
- Understand how dementia can lead to behaviours which may seem challenging or disturbing for that person
Skills:
- To know be able to assess behaviours that challenge to identify a cause
- To feel more confident engagin with people suffering with cognitive impairment to de-escalate situations.
- To know when to use medication and when not to.
Attitudes:
- Engage families and carers in conversation about why these behaviours could be happening
- To consider behaviours that might challenge as an unmet need rather than a challenge per se.
Definitions:
“Dementia is a syndrome – usually of a chronic or progressive nature – in which there is a deterioration in cognitive function (ie the ability to process thought) beyond what might be expected from normal ageing. It affects memory, thinking, orientation, comprehension, calculation, learning capacity, language and judgement. Consciousness is not affected. The impairment in cognitive function is commonly accompanied, and occasionally preceded, by deterioration in emotional control, social behaviour or motivation.”
Practical Definition:
Consciousness can be altered in Dementia with Lewy Body and in the late stages of any dementia, when the pathological changes have affected the whole brain.
These can be called various things: behavioral and psychological symptoms in dementia (BPSD), behaviours that challenge, neuropsychiatric symptoms.
Key Points from Discussion
There are several different types of dementia seen in older adults, each with it’s own particular pattern of cognitive changes. [short recap of series 1 ep 4 Communication in cognitive impairment]
- Alzheimer’s disease is the most common cause, followed by Vascular dementia,
- Other types include Dementia In Lewy-Body, Dementia in Parkinson’s (hallucinations)
- Frontotemporal dementia (early aggression and disinhibition)
- Increasingly alcohol related dementias.
When a person living with dementia starts to experience different or exaggerated behaviours, that would not have been usual for them, it can have a significant impact not just the person with dementia but also their family or carers.
Many of the behaviours which are called “behavioural” symptoms of dementia are not actually symptoms of dementia itself, but are other symptoms/problems which cannot be communicated because of the impact of dementia on language and communication.
Affect up to 90% of people with dementia at some course in their illness, can inlcude
- Agitation: up to 75%
- Wandering: up to 60%
- Depression: up to 50%
- Psychosis: up to 30%
- Screaming/calling out: up to 25%
- Aggression: up to 20%
- Sexual disinhibition: up to 10%
Others: inappropriate urination/defecation, disrobing, perseveration, repetitive questioning, hoarding/hiding, eating inedible objects, resisting to personal care (Cerejeira et al, 2012) (Ref 1)
Cerejeira et al – Behavioral and Psychological Symptoms of Dementia. Frontiers in Neurology 2012
One of the difficult things in an acute medical unit or in an assessment setting is differentiating between Behavioral and psychological symptoms in dementia and a delirium.
Using a case example we will talk through how to work this out and therefore which treatment course to follow, as each has different evidence based options.
Pearl is 85 and is admitted from a care home to the assessment unit. The care home report she is increasingly agitated and is becoming too ‘challenging’ for them to manage. A carer from the home has brought her to the unit. The carer has known her for the last year.
How to approach this:
- What is the ‘problem’ exactly?
- What are the behaviours that challenge?
- How long has this been happening for?
- What triggers it (antecedents)
- What makes it better and what makes it worse?
- What is the course of this?
- Why now?
- What is the relevant past medical and psychiatric history?
- Do they have a known diagnosis of dementia?
- If so what type, what is the stage, are they on any medication treatments?
- Are any other teams involved?
- Has she been seen by the diagnostic memory clinic (if so – there may be a very thorough assessment with details about her personal history)
- What is the relevant personal and social history?
- Is there a This is Me document to give you an understanding of the patient as a person if they are not able to tell you fully?
‘NERD ALERT’??
(Kitwood – personhood, and increasingly towards ethical frameworks of relationality and citizenship)
- What Collateral History is Available from carer, care home, family?
PIECES is a framework that can help to guide approach:
Physical problem or discomfort
- Acute medical problem: delirium
- Drugs (polyphamacy, SEs), alcohol, other substances
- Chronic Disease effects
- Pain – under-recognised and undertreated
- Primitive reflexes
- Basic human needs – tiredness, hunger, thirst
Intellectual or cognitive changes
- Type of demenita
- The As: Anosognosia, Amnesia, Aphasia, Apraxia, Agnosia, Altered perceptions, Apathy
Emotional
- Depression
- Anxiety
- Psychosis
- PTSD of earlier experiences
- Adjustment difficulties
- Interactions with carers (important to identify burnout in carers – acute presentation to services may not actually be due to the behaviour getting worse, but due to carers being worn out, or having their own mental health problems)
- Aggression
Capacities
- Boredom
- Unused energy or previous habits (eg: “wandering”may actually be quite purposeful even if mistimed, or out of sync with other care home routines)
- Anger
- Changes in interest or difficulty keeping up with previous interests
- Demands exceed capabilities (frustration and catastrophic reactions)
Environment
- Relocation, feeling lost, needing to get “home”
- Ambience: excessive or distressing noise, unfriendly, confusing environment, poor lighting
Social and cultural
- Spiritual and cultural needs
- Language (eg: carers not speaking the right language)/PWD returning to previous language
- Family and friends
Back to Pearl…
Pearl is described as “agitated and aggressive”. (The problem) Pearl has become increasing “agitated” during personal care. She seems perplexed by carers washing and dressing her and can strike them telling men in particular to go away. She will only allow females to help her in the bathroom. She can no longer follow simple commands such as lift your leg, step forwards and cannot retain short sentences.
She spends a lot of the day pacing and can be aggressive physically to other residents if they get in her way. She can push other residents out the way and is particularly distressed by the resident in the neighbouring room who is male. Busy periods in the home (visiting times, meal times) result in more agitated behaviour.
Pearl does not sleep well at night and the night staff report she usually sleeps for about 3 hours. She usually gets up and they give her a cup of tea and she paces the day room and corridors. She can fall when she gets tired and has been pacing for more than a few hours.
All of the above has noticed to get gradually worse over the last 6-12 months. In the last week it is noticeably worse, this is possibly triggered by her only daughter going on holiday and not visiting every day. The GP visited and ruled out urinary tract infection.
On clarification she has a diagnosis of Alzheimer’s dementia in the severe stages. She is dependent on carers to meet her basic needs (washing, dressing, continence). She has had Alzheimer’s for about 5 years and has been in a care home for 18 months. At her last memory test (MMSE) she scored 8/30 indicative of severe stages dementia. She has a history also of hypertension and osteoarthritis.
This is Me: Pearl used to work as a nursing sister, predominantly working night shifts at a busy hospital. She has one daughter who is very supportive and visits alternate days that she appears to recognise and appears to enjoy her visits.
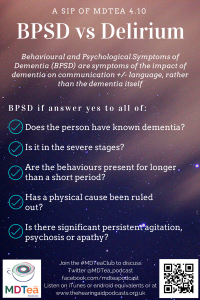
Delirium vs BPSD – answer yes to all of:
> Does the person have a known dementia?
> Is it in the severe stages?
> Are the behaviours present for longer that just a short period?
> Has a physical cause been ruled out?
> Is there significant persistent agitation or psychosis or apathy?
> Has delirium been ruled out?
Back to Pearl.: Pearl has been diagnosed with Behavioral and Psychological Symptoms in Severe stages Alzheimer’s dementia. There is no suggestion of a delirium (an acute confusion). The GP has ruled this out recently.
Cognitive symptoms- Pearl has an MMSE 8/30- severe stages. She can no longer follow simple commands (problems with retention of information (short term memory) and receptive difficulties (understanding of information).
Non-Cognitive Symptoms/behavioural and psychological symptoms. Pearl has agitation, pacing, sleep problems noted. She is more irritable than she was pre-morbidly (change in mood). She is not noted to have psychotic symptoms (delusions and hallucinations). She is not sexually disinhibited.
Assessment
- If not delirium – discharge ASAP – hospital is not a good place for people with dementia
- If not, is there a DAD team at the hospital that can help.
- Find people who can help with the assessment process: Dementia nurses, psychiatrists, psychologists, SALT (in terms of communication strategies), OT (in terms of approaches to personal care and occupational functioning), social workers who can review the package of care (though many of these will be community based)
- Often the assessment process will identify what can be treated/alleviated
- Review medication and medical conditions:
- Is she on activating medications at night?
- Is she in pain and unable to express this?
- Does she have untreated chronic conditions which mean she is uncomfortable a night (eg: arthritis, incontinence).
- Is she depressed?
Non-Pharmacological options
- Day time activity and occupation, reduce boredom especially when daughter away and not able to visit. Using the This is Me or Reach out to me document to personalise this. (or ask daughter what she used to enjoy doing, and consider whether any of this is still possible or can be adapted for her current level of cognition). Could she be taken for a walk during the day. Was she someone who previously liked walking?
- Distraction and behavioural approaches when agitation builds
- Avoid triggers: e.g. busy periods in care home. Pearl may benefit from having meals in a smaller room or arranging ways to keep her main areas low stimulus. Avoid male staff to do personal care and not to have a male resident next to her room as this distresses her. Identify if the staff who are able to manage better are doing anything differently from those who struggle with her. Accept that bathing is not required every day.
- Sleep hygiene. Build in more activity in the day. Avoid caffeinated drinks after 6pm and overnight if she gets up (can use decaf tea). En-courage to go back to bed for periods when wakes and gets up at night to avoid sleep-wake reversal.
- Also be aware that some BPSD will resolve spontaneously – partly due to the disease progression, sometimes due to progressive frailty. If there aren’t risks to self/others or distress associated watchful waiting can also be appropriate.
Pharmacological Approaches (medication)
- Is she already on donepezil?
> Cholinesterase inhibitors may reduce the emergence of BPSD and have a role in their treatment.
Role of donepezil in the management of neuropsychiatric symptoms in Alzheimer’s disease and dementia with Lewy bodies.
Cummings et al CNS neuroscience & therapeutics, 2016
- There is good evidence for Memantine in BPSD in Alzheimer’s Dementia (and mixed). This is available as a tablet and an oral pump and is titrated up against renal function usually over 4 weeks usually in weekly steps.
> It can reduce agitation and aggression
> It can help sleep (it is sedating) so often given at night or in a split dose
> It may help mood symptoms (apathy, low mood, irritability)
>It can help cognitive symptoms (cognitive enhancer)
- Antidepressants may be tried. There is less strong evidence in trials for their use. There is a thought that perhaps depression in dementia is a different phenomenon from depression without cognitive impairment (ie: larger component of apathy which is harder to treat). [covered this in depression episode)
> Citalopram for BPSD (Siddique et al 2009) reduced irritability, apathy and hallucinations but small sample size
Effect of a serotonin reuptake inhibitor on irritability, apathy and psychotic symptoms in patients with Alzheimer’s disease.
The Journal of clinical psychiatry, Siddique et al 2009.
> SSRIs can help with sexual disinhibition due to the sexual side effects.
> Mirtazapine (for the person with dementia) can help carers of those looking after people with in moderate dementia for low mood (HTA- SADD Trial, Banerjee) although it may be as good as watchful waiting for the patient.
Sertraline or mirtazapine for depression in dementia (HTA-SADD): A randomised, multicentre, double bind, placebo controlled trial.
> Trazadone, a sedating antidepressant is sometimes used in divided low doses often for its sedating effect in clinical practice. Although it has limited trial evidence for its use.
> Sleep medications may help in some patients such as Z-drugs (Zopiclone).
> Melatonin showed some efficacy in improving sundowning and agitated behaviour in dementia
Effectiveness of melatonin treatment on circadian rhythm disturbances in dementia. Are there implications for delirium? A systematic review. International Journal of Geriatric Psychiatry. de Jonghe et al 2010
> Effective management of pain has been shown to improve agitation
Efficacy of treating pain to reduce behavioural disturbances in residents of nursing homes with dementia: cluster randomised clinical trial. BMJ. Husebo et al, 2011
- Antipsychotics are used as a last resort for severe and challenging behaviours, severe agitation and or psychosis at very low doses. There has been a huge shift away from the use of antipsychotics in dementia after the black box warnings released by the FDA.
> Low dose risperidone once a day initially
> Stroke risk should be considered (3 in 100), as well as increased falls risk.
An evaluation of six RCTs of risperidone use in patients with dementia has recently been published by Rob Howard and colleagues. It essentially showed that those who have psychotic symptoms such as delusions have lower mortality than those who do not. The implication being that it may be appropriate to use antipsychotics for psychotic symptoms (and actually treating these symptoms is beneficial).
Baseline characteristics and treatment-emergent risk factors associated with cerebrovascular event and death with risperidone in dementia patients. British Journal of Psychiatry. Howard et al, 2016
> Benzodiazepines may be prescribed, usually on an as required basis.
- Short acting Lorazepam orally is preferred at 0.25-0.5mg starting dose (max 2mg/24hrs) at a minimum of 4 hour intervals.
- Additional nursing care may be required after prescription due to the sedating effect (increased falls risk).
- Some patients have a paradoxical reaction and become more agitated with benzodiazepines. In these patients, they are best avoided.
Pearl is started on Memantine by the Geriatrician/Older Persons Mental Health (OPMH) Doctor in the assessment unit. It is discussed with the care home it will take up to 4 weeks to take full effect.
The OPMH nurse practitioner for the assessment discusses with the care home approaches to take to help. He suggests engaging her with some tasks in the day (dusting as she was always house proud, singing as she was always in the choir, church services as she always liked to attend). He discusses distraction techniques to try when she starts to become more agitated. Can check if she is known to the Alzheimer’s society in the local area and see if they can suggest any local activities (eg: Singing for the brain, dementia friendly cinema, chair based exercise)
Pearl’s care plan is altered to only have female staff to provide personal care and it is raised that she may need to move rooms to not be next to a male resident as this distresses her.
The home is recommended to do a Cohen-Mansfield Agitation Inventory 2 weekly to assess the response to the interventions and monitor the impact of these changes. This is a tick box agitation score which can be filled out by a nurse or care worker in the home that knows her.
Pearl stays on the assessment unit for a day but it is agreed it would more conducive for her to be discharged back to the care home as the assessment unit is busy and noisy and will cause her further distress.
The Community Mental Health Team nurse for Older People are requested to review in a few weeks the response to treatment, liaise with the daughter and the care home and ensure the new care plans meet Pearl’s needs.
She does not require DOLS on the assessment unit as she is only admitted for a day. She is already under a DOLs at the care home which is under annual review.
NICE Guidance
Dementia: supporting people with dementia and their carers in health and social care. CG42 – 2016
Curriculum Mapping:
This episode covers the following areas (n.b not all areas are covered in detail in this single episode):
| Curriculum | Area | |
| NHS Knowledge Skills Framework | Suitable to support staff at the following levels:
| |
| Foundation curriculum | Section
1.2 3.10 | Title
Delivers patient centred care and maintains trust Recognises,assesses and manages patients with long term conditions |
| Core Medical Training | The patient as central focus of care
Confusion, Acute / Delirium Aggressive / Disturbed Behaviour Memory Loss (Progressive) | |
| PA matrix of conditions | Dementia | |
| Higher Specialist Training in Geriatric Medicine | 3.2.2 Common Geriatric Problems (Syndromes)
33 Dementia 42. Psychiatry of Old Age 49. Dementia and Psychogeriatric Services | |
| GPVTS program | Section 3.05 – Managing older adults
| |
| ANP (Draws from KSF) | Section 7.21 – Dementia |




