Episode 3.04 Older adult abuse and safeguarding
Presented by:
Dr Iain Wilkinson (Consultant Geriatrician East Surrey Hospital)
Dr Jo Preston (Consultant Geriatrician St George’s Hospital)
Jackie Lelkes (Social Work Lecturer at University of Brighton)
Dr Tapiwa Moffatt (Clinical Fellow, East Surrey Hospital)
David Flood (Adult Safeguarding Lead, St George’s Hospital)
Broadcast date: 28th March 2017
Click here for a PDF version of the infographic
CPD log
Click here to log your CPD online and receive a copy by email.
Episode 3.04 Older Adult Abuse and Safeguarding – Show Notes
Click here for a PDF version of the show notes.
Learning Outcomes
Knowledge:
- To understand the term vulnerable adult
- To understand the signs and symptoms of adult abuse
- To understand the legal framework for safeguarding a vulnerable adult
Skills:
- To recognise a vulnerable adult
- To understand the process of reporting adult abuse
Attitudes:
- To understand that everyone has a responsibility to identify an older person at risk of abuse
- To understand that everybody has a responsibility to report abuse, whether actual or suspected
Definitions:
Action against Elder Abuse Definition:
“Elder abuse is a single or repeated act, or lack of appropriate action, occurring within any relationship where there is an expectation of trust, which causes harm or distress to an older person.”
This type of violence constitutes a violation of human rights and includes physical, sexual, psychological, emotional; financial and material abuse; abandonment; neglect; and serious loss of dignity and respect.
Key Points from Discussion
The scope of the problem
Older people are particularly vulnerable to abuse
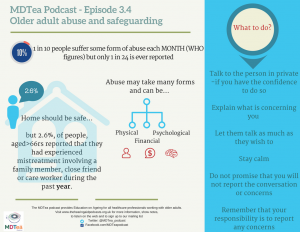
- Worldwide approximately 1 in 10 older people experience abuse each month (WHO). According to AEA, over 500, 000 older people are abused each year in the UK. Likely to be an underestimate because only approx.
- 1 in 24 cases of elder abuse is reported- older people often afraid to report cases of abuse to family, friends, or to the authorities.
- Older people with dementia are at special risk- as many as 2 in 3 have been abused (WHO)
- Women over 70 who are dependent, frail and alone are particularly vulnerable.
Although rigorous data are limited, a study provided prevalence estimates of the most common types of abuse in high- or- middle-income countries:
- physical abuse: 0.2-4.9%;
- sexual abuse: 0.04-0.82%;
- psychological abuse: 0.7-6.3% (based on substantive threshold criteria);
- financial abuse: 1.0-9.2%; and
- Neglect: 0.2-5.5%.
There is a prevalence of psychological abuse, usually through intimidation or coercion linked to financial abuse.
Perpetrators of abuse or neglect are often people who are trusted and relied on, such as family members or care staff.
Institutional abuse: Not much data. A survey of nursing-home staff in the United States of America, suggested rates may be high:
- 36% witnessed at least 1 incident of physical abuse of an elderly patient in the previous year;
- 10% committed at least 1 act of physical abuse towards an elderly patient;
- 40% admitted to psychologically abusing patients.
Crimes against older people often take place in a context of abuse and mistreatment.
A UK study in 2007 showed that 2.6%, of people, (about 227,000) aged 66 and over living in private households reported that they had experienced mistreatment involving a family member, close friend or care worker during the past year.
Over half of situations of abuse involved partners.
- This is often in the context of people who may be frail and unwell themselves and struggling to provide care
- When include incidents involving neighbours and acquaintances, the overall figure increases to 4.0% of people aged 66 and over.
- This adds up to 342,400 older people in the UK who are subject to some form of mistreatment each year.
This is just data for people living at home – older people can experience crime in many other places
Risk factors
(Quoted from the WHO Factsheet)
Anyone can be at risk but some examples of people who might be at risk include:
- Someone who is frail due to ageing
- Someone with a serious health condition
- Someone with a physical disability
- Someone with a visual disability
- Someone with a hearing impairment
- Someone who has memory problems or dementia
- Victims of domestic violence
- Someone with a mental health difficulty
- Someone with a learning disability
Individual
Risks at the individual level include poor physical and mental health of the victim, and mental disorders and alcohol and substance abuse in the abuser. Other individual-level factors, which may increase the risk of abuse, include gender of victim and a shared living situation. While older men have the same risk of abuse as women, in some cultures where women have inferior social status, elderly women are at higher risk of neglect and financial abuse (such as seizing their property) when they are widowed. Women may also be at higher risk of more persistent and severe forms of abuse and injury.
Relationship
A shared living situation is a risk factor for elder abuse. It is not yet clear whether spouses or adult children of older people are more likely to perpetrate abuse. An abuser’s dependency on the older person (often financial) also increases the risk of abuse. In some cases, a long history of poor family relationships may worsen as a result of stress when the older person becomes more care dependent. Finally, as more women enter the workforce and have less spare time, caring for older relatives may becomes a greater burden, increasing the risk of abuse.
Community
Social isolation of caregivers and older persons, and the ensuing lack of social support, is a significant risk factor for elder abuse by caregivers. Many elderly people are isolated because of loss of physical or mental capacity, or through the loss of friends and family members.
Socio-cultural
Socio-cultural factors that may affect the risk of elder abuse include:
- depiction of older people as frail, weak and dependent;
- erosion of the bonds between generations of a family;
- systems of inheritance and land rights, affecting the distribution of power and material goods within families;
- migration of young couples, leaving elderly parents alone, in societies where older people were traditionally cared for by their offspring;
- Lack of funds to pay for care.
Within institutions, abuse is more likely to occur where:
- standards for health care, welfare services and care facilities for elder persons are low;
- where staff are poorly trained, remunerated, and overworked;
- where the physical environment is deficient; and
- Where policies operate in the interests of the institution rather than the residents.
Safeguarding
There are no eligibility criteria. However an adult who needs safeguarding is:
- An adult who has care and support needs (whether or not the local authority is meeting any of those needs); and
- Is experiencing or at risk of, abuse or neglect; and
- Because of those needs is unable to protect themselves from either the risk of or the experience of abuse or neglect.
This definition means that the Local Authority, under the Care Act, 2014, have a duty to follow up any reported concerns regardless of whether there is actual evidence or a suspicion that the person may be subject to abuse.
The statutory guidance enshrines six principles of safeguarding:
- Empowerment – which is the presumption that the person is best placed to lead the decision and to give informed consent to the investigation or outcomes from the investigation unless they lack mental capacity
- Prevention – better to take action before the harm/abuse occurs
- Proportionality – the response to the allegation of abuse should be proportionate and the least intrusive response appropriate to the risk presented
- Protection – support should be given to those in greatest need
- Partnership – solutions should be found locally working with the persons community
- Accountability – safeguarding should be delivered in an accountable and transparent way. (Show your working/documentation and have a named person etc. Will talk to the accused and person on receiving end)
Together these principles shift the way an individual is safeguarded to a person-centred approach, with the aim of achieving the outcomes the person wants.
It is important to remember that abuse can happen anywhere, for example in a persons own home, a care home or residential home, a hostel, in supported living, in homes where people have shared living arrangements or in hospital.
Types of abuse
The Care Act, 2014, identifies 10 categories of abuse, for all the categories, many of the indicators that abuse may be occurring are well known, but some may be less understood or obvious. The list below is now exhaustive and it is important to remember that an individual can be subject to more that one area of abuse at any one time.
- Physical abuse, which includes hitting, punching, scalding, involuntary isolation, or confinement, misuse of medicine, forcible feeding or withholding food and unauthorised restraint. Signs that a person may be subject to physical abuse include no clear explanation for their injury, which are not consistent with their lifestyle. They are frequently injured, or have unexplained falls and medical treatment has not been sought.
- Domestic violence or abuse is when a person is subject to controlling, coercive, or threatening behaviour or violence between individuals over 16 years who are or have been involved in a sexual relationship. Domestic violence also includes ‘honor-based’ violence, female genital mutilation, and forced marriages. A person my present with low self esteem, physical evidence they have been abused, being isolated from friends and family. They may indicate that they believe the abuse is their fault
- Sexual abuse, includes rape or attempted rape, inappropriate touching anywhere, any sexual activity the person cannot consent to, sexual photography or forced used of pornography. Indicators that a person may be experiencing sexual abuse, includes bruising, particularly to the thighs, buttock’s and upper arms. Bleeding, infections, pain, sexually transmitted disease or itching in the genital region. Excess fear or withdrawal from a relationship. Self-harming.
- Psychological or emotional abuse – types of abuse can include enforced social isolation, removing mobility or communication aids, preventing somebody meeting their religious of cultural needs, harassment, bullying, cyber bullying. Suspicion raised if a person appears withdrawn or there is a change in their psychological state in the presence of another person. The person has low self-esteem, demonstrates signs of distress for example being tearful.
- Financial or material abuse – theft of money or possessions, fraud, preventing a person accessing their own money or assets, arranging less care than is needed to save money to maximise inheritance, moving into a persons home rent free and/or under duress. Indicators may include an unexplained lack of money to maintain their lifestyle, recent changes in deeds or title to a property, failure to provide receipts for shopping or financial transactions undertaken on the person’s behalf. Obtaining a LPA after the person is assessed as lacking mental capacity to manage finances.
- Modern Slavery – forced labor, domestic servitude. Indicators may include signs of physical or emotional abuse, seeming to be under the influence of another person, lack of personal effects, appearing hesitant to talk to strangers.
- Discriminatory abuse includes unequal treatment based on age, disability, gender reassignment, marriage and civil partnership, pregnancy and maternity, race, religion and belief, sex or sexual orientation – all protected characteristics under the Equality Act 2010. Other indicators include verbal abuse, denying a person their basis rights to healthcare. The person may appear as withdrawn and isolated, angry or frustrated, be fearful of anxious.
- Organisational or institutional abuse applies to such settings as nursing and residential homes and hospital, within this category you may be concerned if an organization discourages visits or the involvement of relatives, there is an authoritarian management, or there is insufficient staff or a high turn over of staff. There is a lack of respect for dignity and privacy for example the person’s dignity is not maintained during bathing or toileting. Medication is being misused or there is an absence of an up to date care plan.
- Neglect or acts of omission. Concern would be raised if the person is denied access their basis needs including food, shelter, clothing, heating, personal and medical care. If medication is not administered appropriately or care is provided in such a way, that he person dislikes. The person may present as malnourished, or have untreated medical conditions or injuries; they may have pressure sores, which have not been treated.
- Self-neglect is when a person fails to care for their personal hygiene and their behaviour impacts on their safety. They may be living in squalid or unsanitary conditions or be very unkempt. It may be that they are hording either possessions or animals. They may be non-compliant with health and social care.
Evidence or suspicion of any one of the above indicators should not be considered as evidence that is occurring, but should alert any health care or social care practitioner that further assessment should be undertaken.
At a glance 69: Adult safeguarding Types and Indicators of abuse
What to do if you suspect it
In order to respond appropriately where abuse or neglect may be taking place, anyone in contact with the adult, must understand their responsibility and have access to advice, support and practical and legal guidance, including understanding local inter-agency policies and procedures.
All organisation’s have policies and procedures or agreed ways of working, which give guidance on prevention and procedures to follow if and when abuse or neglect has happened or is suspected. Your manager or a senior member of staff should always be your point of contact for any questions or concerns you might have.
If you are worried, that someone is experiencing abuse of neglect. What should you do?
- Talk to the person in private, if you have the confidence to do so
- Explain what is concerning you i.e. loss of weight, the person has become withdrawn.
- Let them talk as much as they wish to. Be aware they they may find it difficult to talk, for fear of escalating the situation or they may be subject to coercion.
- Stay calm; regardless of what you are hearing; by becoming upset yourself it is likely the person will stop talking.
- Do not promise that you will not report the conversation or concerns.
- Remember that your responsibility is to report any concerns it is then the responsibility of LA to decide if they will undertake a safeguarding enquiry.
- Ask then what they would like to happen and inform them of the help available
Findings from serious case reviews have sometimes stated that if professionals or other staff had acted upon their concerns or sought more information, then death or serious harm might have been prevented.
Legal Mandate
Care Act 2014
- Came into force Dec 2015
- The Care Act works on the principle of ‘well-being’, which the Act describes as being related to:
- Personal dignity (including treating the individual with respect)
- Physical and mental health and emotional wellbeing
- Protection from abuse and neglect
- Control by the individual over day-to-day life (including over care and support provided and the way it is provided)
- Participation in work, education, training or recreation
- Social and economic wellbeing
- Domestic, family and personal wellbeing
- Suitability of living accommodation
- The individual’s contribution to society.
- Prior to this no law specifically dealt with safeguarding adults at risk of abuse or neglect, statutory guidance was located within “No Secret’, 2000.
- The Care Act says that local authorities are the lead safeguarding agencies. However, they can ask other agencies to undertake the safeguarding enquiry on their behalf. It is important the LA work with their partner organisations – including housing, the NHS and the police – to ensure that adults who may be at risk of abuse or neglect are enabled to live as safely and independently as possible, making their own decisions and taking control of their own lives.
- Others i.e. police, health services and individual health professionals, including GPs, have a duty to cooperate and have a vital role to play in preventing, reporting and responding to allegations of abuse or neglect.
-
- Everyone needs to be involved in supporting the recovery of adults who have been victims of abuse, as well as working with those who are abusive.
- The Care Act also places a duty on the LA to safeguard carers, who can equally be at risk of abuse.
- Place a duty on councils to fund advocacy for people who are ‘unbefriended’ i.e. do not have anyone – family/friends to support or speak up for them, or if the safeguarding allegation is against the person who would normally support them and would find it difficult to be fully involved without support.
In line with the Human Rights Act 1998:
- Article 3: Right not to be subject to torture, inhuman or degrading treatment. Treatment may be degrading if it ‘humiliates or debases an individual showing a lack of respect for, or diminishing his or her human dignity or arouses feelings of fear, anguish or inferiority capable of breaking an individual’s moral and physical resistance
- Article 8: Right to enjoy private and family life without interference from authorities
- Article 6 entitles everyone to a ‘fair hearing’ when a decision is made about their civil rights and obligations. This includes the right to be consulted before decisions are made, and to be given reasons for decisions
- Duty to protect: Public authorities have a proactive duty towards adults at risk to take “reasonable steps to prevent ill-treatment of which the authorities had or ought to have had knowledge.’
Local authorities and courts as public bodies have a duty to consider Human Rights when making decision about an individual’s welfare. Where rights are conflicting they must strike a balance and act proportionately- find the least restrictive option for the individual.
The emphasis is on sensible risk appraisal, not risk avoidance, taking into account an individuals’ preferences, histories, circumstances and life-styles to achieve a level of acceptable risk. As Lord Justice Munby said: “what good is it making someone safer if it merely makes them miserable?”
What if a crime has been committed?
Many of the types of abuse mentioned are also a crime
- Assault
- Sexual assault or rape
- Neglect or willful neglect of a person without mental capacity to care for themselves
- Unlawful imprisonment- not as dramatic as it sounds- may just be as simple as restriction of movement – links to the importance of having a deprivation of liberty safeguarding authroisation if the person is to be legally deprived of their liberty.
- Theft
- Fraud
- Domestic violence
Psychological abuse – controlling or coercive behavior (since Dec 2015)
If it is believed a crime has been committed it is the role of the police to lead the investigation, and if necessary interview the alleged victim, perpetrator and witnesses.
It is important to remember that Safeguarding an older person is complex, The Care Act balancing the right to be safe with the right of the individual to make informed choices, whilst ensuring that the person’s wellbeing is promoted including, taking into consideration their views, wishes, feelings and beliefs when deciding on any course of action.
Resources
If you have some links or resources you’d like to share, get in touch and we’ll add them here. Twitter @MDTea_podcast Facebook www.facebook.com/MDTea or email thehearingaidpodcasts@gmail.com
Curriculum Mapping: This episode covers the following areas (n.b not all areas are covered in detail in this single episode):
| Curriculum | Area |
| NHS Knowledge Skills Framework | Suitable to support staff at the following levels:
Personal and people development level 1-3 Health, Safety and Security level 1-3 Service improvement level 1 |
| Foundation Curriculum 2012 | 2.1 Treats patient as centre of care
4.2 Legal framework of medical practice 6.1 Lifelong learning 6.2 Evidence and guidelines 7.1 Makes patient safety a priority in good clinical practice 10.2 Supporting patient decision making |
| Foundation Curriculum 2016 | 2. Patient centred care
3. Protection of vulnerable groups 4. Self-directed learning 6. Interface with other healthcare professionals 11. Clinical management 19. Patient safety |
| Core Medical Training | Common competences:
System specific competences:
|
| GPVTS program | Section 3.05 – Care of older adults
|
| ANP (Draws from KSF) |
Section 20. The patient as central focus of care Section 25 Legislation Section 26 & 27 Communication |
| PA Matrix of conditions | Conditions in Category 1B:
1.5.3 Child/elder abuse |
Feedback We will add feedback to this as we receive it! The website will have the most up to date version always available: www.thehearingaidpodcasts.org.uk/mdtea Find Us! To listen to this episode head to our website, itunes or stitcher. Give us feedback by emailing us, via twitter or facebook. Check out our cool infographic A sip of… summarising 5 key points on topic. It’s made for sharing!





