Episode 3.07 Community Interface
Presented by:
Dr Iain Wilkinson (Consultant Geriatrician East Surrey Hospital)
Dr Jo Preston (Consultant Geriatrician St George’s Hospital)
Dr Amy Heskett (Community Geriatrician, West Kent)
Alison Fitzgerald (Nurse, OPAL Team Leader St George’s Hospital)
Broadcast date: 9th May 2017
Click here for a PDF version of this infographic
Broadcast date: 9th May 2016
CPD log
Click here to log your CPD online and receive a copy by email.
Episode 3.07 Show Notes Community Geriatrics
Click here for a pdf version of these notes
Learning Outcomes
Knowledge:
- To understand different types of hospital at home services and how they work
- To recall the factors which may influence adverse outcomes in either hospital or home environments, e.g. delirium, hydration.
Skills:
- To recognise when someone can be treated at home Vs admission to hospital.
- To balance the risks of home treatment and hospital admission, as a professional working in either environment.
Attitudes:
- To consider whether the person in front of you can be managed at home.
- To be person centred in decisions regarding home treatment
Social Media Spots this week
National Osteoporosis Guideline Group new guidelines are out and are here. NEW NOGG guidelines
Wenurses – tweeting for revalidation
Emergency medicine cases podcast- really good episode on UTIs
Definitions:
Rather than a specific definition it may be better to think about aims of the services (see below). Some terms you may hear about are:
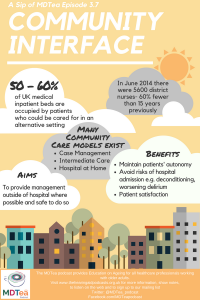
- Hospital at Home: community- based provision of services usually associated with acute inpatient care.
Defining and disseminating the hospital-at-home model, Leff, CMAJ 2009
- Intermediate Care: Intermediate care services are provided to patients, usually older people, after leaving hospital or when they are at risk of being sent to hospital. The services offer a link between places such as hospitals and people’s homes, and between different areas of the health and social care system – community services, hospitals, GPs and social care.
National Audit of Intermediate Care 2014
- Case Management: a collaborative process of assessment, planning, facilitation and advocacy for options and services to meet an individual’s health needs through communication and available resources to promote quality cost-effective outcomes (Case Management Society of America 2010).
Practical Definition:
All of these services aim to provide management outside of hospital where possible and safe to do so. The scope of what the provide can be quite wide though from: a full hospital at home service with intravenous antibiotics etc. to services more focused on other aspects including advance care planning. They all though avoid paternalism and the risks associated with hospital admission.
Review of literature
For any service to be effective it needs to be multidisciplinary and responsive.
- Occupational therapy is an example of a key profession to integrating the health and social care services needed to enable people to achieve their wellbeing outcomes (Reducing Pressures on hospitals – report by College of Occupational Therapy)
Who is at risk of admission to hospital (and hence who may have the most to gain from community interface services?
-
Those under 5 years old or over 85.
- Those from socio-economically deprived areas (up to 90% more likely to have unplanned admission in GP practices in most vs least deprived areas.
- People with high levels of morbidity and chronic illnesses (independently)
Avoiding hospital admissions. What does the research say? Purdy 2010, Kings Fund publication
There is increasing recognition of the interdependence between hospital and community-based health and social care services, particularly for those who are frail and/or suffer from long-term conditions.
- 50 – 60 per cent of medical inpatient beds are occupied by patients who could be cared for in an alternative setting and a significant proportion of these are older adults with frailty and / or long term conditions.
- There is evidence that proactive care and supported rehabilitation and discharge could reduce length of stay and deliver better patient experience.
- The key to reducing the use of acute beds lies in changing ways of working
across a system, including changes within hospitals, rather than piecemeal
initiatives.
See table 2 from Reconfiguration of clinical services – Kings Fund 2014
Using hospital admissions and / or financial endpoints in evaluations as they do not show the whole picture.
Even with successful implementation, there is little evidence to suggest that more community-based models of care will generate significant savings. Future workforce projections also present challenges to community-based models of care.
Sheppard et al have reviewed the evidence for hospital at home services. There are a small number of studies which give weak evidence and a short follow up time. The same authors are currently recruiting to a large trial on hospital at home services.
Evidence for quality
- There is strong patient satisfaction associated with virtual ward programmes and case management programmes
- Available evidence points to a positive impact of integrated care programmes on the quality of patient care and improved health or patient satisfaction outcomes.
- Evidence from a randomised controlled trial indicated that patients were more satisfied with ‘hospital at home’ than with inpatient care because it was possible to provide a more personal style of care and staying at home was considered to be more therapeutic.
Reconfiguration of clinical services – Kings Fund 2014
We then talked through a case example with Dr Amy Heskett (Community geriatrician – Kent, UK) and Alison (OPALS nurse St George’s Hospital, Tooting, London) with a focus on practical considerations regarding looking after an older person in their own home.
| Curriculum | Area | |
| NHS Knowledge Skills Framework | Suitable to support staff at the following levels:
|
|
| Foundation curriculum (2016) | Section
1.2 Patient centred care 1.4 Self directed learning 2.7 Interaction with colleagues 3.9 Recognises, assessesand initiates management of the acutely ill patient |
|
| Core Medical Training | Confusion, Acute / Delirium
Personal behaviour (Be able to provide specialist support to hospital and community based services) Management of long term conditions and promoting self-care Management and NHS structure (Describes in outline the roles of primary care, including general practice, public health,community, mental health, secondary and tertiary care services within healthcare) Geriatric Medicine |
|
| GPVTS program | Section 2.03 The GP in the Wider Professional Environment
Section 3.05 – Managing older adults
|
|
| ANP (Draws from KSF) | Section 6
Section 7.1 Section 10 Section 11 |
|





1 Response
[…] 3.07: Community Interface […]