Episode 2.3 – Bone Health
MDTea Episode 2.3 – Bone Health
Presented by: Jo Preston (Consultant Geriatrician at St George’s Hospital) and Iain Wilkinson (Consultant Geriatrician at East Surrey Hospital).
Core Faculty: Sarah Jane Ryan, Physiotherapist and Pam Tangmar, Physician Associate.
Guest Faculty: Alun Cooper, GP
In this episode we talk about bone health, what osteoporosis is, what can be done to prevent or minimise it and the associated risks of fractures.
Broadcast date: 27th September 2016
The show notes for this episode will follow shortly.
 Here is a sip of this episode’s MDTea….
Here is a sip of this episode’s MDTea….
Downloadable show notes are here.
CPD log
Click here to log your CPD online and receive a copy by email.
Show Notes Episode 2,3
Learning Outcomes
| Knowledge |
|
| Skills |
|
| Attitudes |
|
Definition of Osteoporosis
“Osteoporosis is a disease characterised by low bone mass and structural deterioration of bone tissue, with a consequent increase in bone fragility and susceptibility to fracture.”
Osteoporosis: assessing the risk of fragility fracture. NICE Guideline 146. August 2012
From a practical point of view:
- Its when someone develops ‘brittle’ bones.
- Healthy bones require a balance between Osteoclasts (cut out bone) and osteoblasts (build up bone) – this process is modulated by PTH and vitamin D metabolism.
- Vit D deficiency is called osteomalacia and that leads to a reduced bone density (often quite rapidly corrected with Vitamin D replacement) – See your local guidelines as to how to do this as it varies slightly from palace to place.
- As we age the bone density reduces gradually from the peak bone mass (in 30s) in women much more rapidly following menopause.
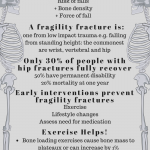
A really key point is to spot when a bone breaks when it should not. This is a a fragility fracture – a good rule of thumb is a low impact fracture should not lead to a large bone fracture e.g. a fall from standing height to the same level leading to a fracture of: hip, pubic rami, rib, vertebra etc.
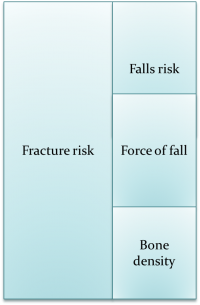
- Fracture risk really is the sum of your patients falls risk, their bone density and the force of the fall. So they may well have a good bone density but may still fracture if they fall a lot, or have a lot of force in the fall (e.g falling down a step or off a chair). Management of a patients fracture risk therefore needs an interlinked falls assessment (go check out Episode 1.5 and 1.9 for some tips on this.. also more is coming in series 2).
Osteoporosis
Osteoporosis is a large health service issue world wide leading to around 9 million fragility fractures per year!
Fragility fractures cause significant morbidity and may lead onto:
- substantial pain and severe disability,
- reduced quality of life,
Hip and vertebral fractures are also associated with decreased life expectancy. The majority of hip fractures need surgery to repair the fracture and 50% of patients are left with a permanent disability. A recent poster we talked about in the MDTea and CAKE (here) talked about the quality of life of patients following surgery. At 30 days patients rated their QOL worse than being dead (this did though improve at 120 days).
When to think about fracture risk?
Consider risk of fracture in all women over 65 and men over 75.
- Have it in your peripheral field of vision for all encounters with these groups e.g. physio appointment, GP, whole MDT e.g. measuring height, falls risk etc.
- Extra thought in high risk encounters e.g. pd clinic,
For those less than 65 years old be aware of the increased risk factors:
- previous fragility fracture,
- current use or frequent recent use of oral or systemic glucocorticoids,
- history of falls,
- family history of hip fracture,
- other causes of secondary osteoporosis (hyper PTH, cushing’s, coeliac etc.)
- Long term PPI have been implicated in an increased fracture risk.
Once you have identified patients as being at risk a quantitative risk assessment is useful (FRAX and Qfracture are examples).
Bone Scan
Some patients will go on to have a bone scan. This is simple and quite cheap to do – patients do need to be able to lie still and get on and off the table though – so just think about their level of mobility before referring them.
A bone scan will give you a T or Z score. A T score is the number of standard deviations from the mean (average) bone mass of a cohort of pre-menopausal women.
Osteopenia = T score of -1 to -2.5
Osteoporosis = T score of <-2.5 – in 2 sites (e.g at the lumber spine and hip).
Treatment
Once you have made a diagnosis treatment of some type is likely to be recommended.
There are things we can all do to help our patients manage their bone health.
- Lifestyle recommendations:
- Reduce alcohol intake (it’s toxic to the bones)
- Ensure calcium and vitamin D intake are sufficient – these may need to be supplemented.
- There is a calcium calculator online (here) so calculate dietary intake to see if supplements needed.
- Greater milk intake was associated with lower bone turnover and higher BMD (link below)
- Stopping smoking
- Exercise
- this needs to be load bearing (so swimming and cycling whilst good exercise are not helpful for your bones.
- Even in older life exercise can lead to a plateauing of the natural bone loss
- Introduce the exercise gradually and move up to a dose of around 2 to 3 times per week.
- In addition in our patients think about that falls risk / recent immobility (it leads to bone loss) / malnutrition and calcium absorption
Physiotherapy assessment
There are some specific things that we can do during a therapy assessment:
- Posture and range of movement – serial height measurements / measure curvature of spine
- Muscle strength and endurance
- Aerobic capability e.g TUG or 6 m walk test
- Balance eg functional reach (thinking about falls risk)
- Pain and Function
Drug Treatment
All drug treatments assume that the patient’s Vitamin D and calcium is replete – so replace these first. There are a good variety of preparations out there so find the one that suits your patients (soluble, chewable, caplets (can go in blister packs)).
Initial treatment:
- Standard initial treatment is bisphosphonate (antiresportive) tablet – these work on reducing the function of Osteoclasts
- Alendronic acid or Risedronate sodium.
- Variable persistence with medications (up to 50% stop taking treatment in one systematic review of trials)
- This can be improved with follow up soon after starting to check for problems.
Both need to be taken weekly for at least 3 years and then reassessed – although again check your local and national guidance for this.
Some points on taking both of these:
- Associated with significant GI upset.
- Improved by following administration guidelines… 30 mins before food, first thing in the morning, stay mostly upright after.
For people that cannot tolerate the oral treatments – or have failed on them there are three injectable treatments that might be suitable – you will have local policies on who, when and how to use these.
- Intravenous bisphosphonate – usually given yearly.
- Denosumab – a monocolonal antibody treatment given as a sc injection every 6 months (A video about how it works is here)
- Teriparatide – This is Parathyroid hormone and is given as a regular self administered sc injection. It increases bone density – the only treatment to really do this – but it is expensive and there will be specific local prescribing guidelines. (A video about this one is here)
NICE technology assessment for second line treatments
Curriculum Mapping:
This episode covers the following areas (n.b not all areas are covered in detail in this single episode):
| Curriculum | Area |
| NHS Knowledge Skills Framework | Suitable to support staff at the following levels:
|
| Foundation Curriculum 2012 | 2.1 Patient as centre of care
7.9 Interface with different specialities and other professions 10.1 Long-term conditions 10.3 Nutrition |
| Foundation Curriculum 2016 | 2. Patient centred care
4. Self-directed learning 6. Interface with other healthcare professionals 10. Support for patients with long term conditions 10. Nutrition |
| Core Medical Training | Common competences:
Symptom based competences:
System based competences:
Bone disease: osteoporosis and osteomalacia
|
| GPVTS program | Section 2.03 The GP in the Wider Professional Environment
Section 3.05 – Managing older adults
|
| ANP (Draws from KSF) | Section 7.10 Falls, fractures and other injuries
Section 7.19 Arthritis, polymyalgia rheumatica, osteoporosis |
| Physician Associate | Conditions in category 1A – 5.10.2 Osteoporosis |




