Episode 2.09 – Falls Prevention
MDTea Episode 2.09 – Falls Prevention
 In this episode we will cover the evidence base for falls prevention, particularly community based programmes designed to improve balance and mobility
In this episode we will cover the evidence base for falls prevention, particularly community based programmes designed to improve balance and mobility
Broadcast date: 13th December 2016
Presented by: Jo Preston (Consultant Geriatrician at St George’s Hospital, London) and Iain Wilkinson (Consultant Geriatrician at East Surrey Hospital).
Core Faculty: Sarah Jane Ryan (Physiotherapy Lecturer at University of Brighton)
Guest Faculty: Alun Cooper (GP in Surrey and Clinical Lead for Fracture Liaison Service in Crawley) and Amy Heskett (Community Geriatrician in Kent).
CPD log
Click here to log your CPD online and receive a copy by email.
Episode 2.09: Falls prevention – Show Notes
You can download these show notes here.
Learning Outcomes
Knowledge:
- To understand the role of falls prevention programmes and their potential
- When to perform a falls risk assessment
Skills:
- Identify the components of a falls risk assessment
- Be able to perform a basic timed ‘up and go’ test
Attitudes:
- To appreciate that falls are a symptom and not a diagnosis in themselves
- Understand that falls may lead to a fear of falling
Definitions:
- The definition of falls is covered in Episode 1.5 Falls – Acute Management
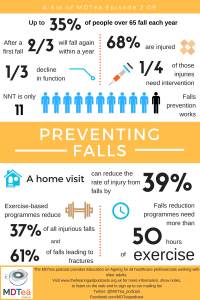
The scale of the problem
- 28-35% of people >65 years old fall each year
- 68% of these had an injury and 24% of these injuries required intervention from a healthcare professional
- 35% of those who have a fall have a subsequent decline in function
- this may affect someone’s ability to stay within their own home, to manage without carers or indeed their chance of enjoying activities.
- After a first fall people have a 66% chance of having another fall within a year.
Falls prevention programmes do work
- NNT (number needed to treat) to reduce falls from strength and balance training is only 11.
- Group and home-based exercise programmes, and home safety interventions reduce both rate of falls and risk of falling.
- Multifactorial assessment and intervention programmes reduce rate of falls but not risk of falling; Tai Chi reduces risk of falling.
- Overall, vitamin D supplementation does not appear to reduce falls but may be effective in people who have lower vitamin D levels before treatment.
Interventions for preventing falls in older people living in the community.
Key Points from Discussion
Falls risk assessment
A recent (2016) article in the BMJ reviewing falls prevention in community dwelling older people highlights that falls result from interactions between multiple individual and environmental risk factors – for example:
- Frailty
- Polypharmacy
- Gait and balance
- Co-morbid conditions
Extensive research has identified many risk other factors in older people in the community, including:
- Previous falls
- Pain – e.g. lower limb or foot
- Cognitive impairment – reduction in verbal ability, processing speed and immediate memory
- Urinary incontinence – rushing to the toilet at night
Key point: You may not think of yourself as someone who ‘sees patients that fall’ (eg podiatry, continence services etc.) but in reality patients may present to a number of different services, and you may be the person that triggers the more detailed assessment. The management of older people is multifactorial and needs Comprehensive Geriatric Assessment.
The BMJ paper suggested a strategy for falls risk assessment based around:
1) History and examination
2) Drug review – involve the patient’s GP and/or pharmacist here
3) Specific review of medical risk factors:
- Vision
- Syncope
- Cardiovascular
- Cerebrovascular
- Diabetes
4) Functional and mobility assessment
5) Psychological effects of the fall
- May reduce mobility to decrease risk of fall but this may cause muscle weakness and joint stiffness
- It is therefore important to encourage or develop techniques to assist with coping with anxiety.
Essentially a CGA! (See episode 1.01- CGA)
Prevention of falls in older people living in the community
Falls prevention exercise programmes
A systematic review provides evidence that fall prevention exercise programmes for older people not only reduce the rates of falls but also prevent injuries.
- The protective effect seems most pronounced for the most severe fall related injuries: estimated reduction is 37% for all injurious falls, 43% for severe injurious falls, and 61% for falls resulting in fractures.
- Many of the risk factors for falls injuries are similar. These factors are correctable by well designed exercise programmes, even in the very old and frail.
- All exercise programmes that have proved to be effective for fall prevention (and all trials included in this review) emphasise balance training, and there is now ample evidence that this improves balance ability. However, most programmes are multi component—that is, also include other types of exercise such as gait and functional training, strengthening exercises, flexibility, and endurance.
- There is evidence that these types of interventions can improve reaction time, gait, muscle strength, coordination, and overall physical functioning as well as cognitive functions, especially executive function.
- It is therefore thought that exercise prevents injurious falls not only by improving balance (e.g Tai Chi and Otago) and decreasing the risk of falling, but also by improving cognitive functioning, and the speed and effectiveness of protective reflexes (such as quickly extending an arm or grabbing nearby objects) or the energy absorbing capacity of soft tissues (such as muscles), thereby diminishing the force of impact on the body.
Systematic review of falls prevention programs
Otago home exercise programme
Administered to 1000 people living at home, aged 65-97. Falls reduced equally in men and women and by 35% overall.
Highest impact was seen in those >80yrs with a previous fall.
- The programme was designed specifically to prevent falls. It consists of a set of leg muscle strengthening and balance retraining exercises progressing in difficulty, and a walking plan.
- The exercises are individually prescribed and increase in difficulty during a series of five home visits by a trained instructor.
- Each person receives a booklet with instructions for each exercise prescribed and ankle cuff weights (starting at 1kg) to provide resistance for the strengthening exercises.
- The exercises take about 30 minutes to complete. Participants are expected to exercise three times a week and go for a walk at least twice a week.
- Support and motivation program is provided alongside.
- Participants record the days they complete the programme and the instructor telephones them each month between home visits.
- Follow-up home visits are recommended every six months.
- This is echoed by the AGILE guidelines which recommend:
- Exercise programmes to reduce falls should be high dose (> 50 hours over 6 months)
- Exercise programmes to reduce falls should have a high balance challenge component.
- They also make the point that people at risk of falling should be asked if they can get up from the floor – and if not be taught strategies to do this.
Consider a home visit
A RCT of 842 houses showed that modifications to a home reduced the rate of injuries from falls by 39% compared with those on a waiting list control group.
Home environment assessment checklists are available,and they are designed to identify:
- Environmental hazards that can be removed or avoided, including tripping obstacles such as cords, rugs, and furniture; slippery surfaces; and poorly illuminated areas
- Accessories that can be installed and furniture that can be modified to facilitate transfer or walking including ramps, proper height toilet seats and beds, grab bars next to the toilet and shower, and railings along walking pathways
- The need and opportunities for use of assistive gadgets and devices, such as extended reaching gadgets, falls monitoring devices, medical staff or rescue alert systems.
Home modifications to reduce injuries from falls in the home injury prevention
intervention (HIPI) study: a cluster-randomised controlled trial.
Keall et al. 2015
Assessing balance
There are many different tests but the two detailed in this episode are:
- Timed Up and Go (TUG) test
This is a useful test as it can easily be done in someone’s home. Measure time taken to rise from a chair, walk 3m, turn around and navigate back to the original starting chair.
- TUG time > 12 seconds is associated with an increased risk of falls.
- Sensitivity 80%
- Specificity 100% – a good test to identify those unlikely to fall
2. 180 degree turn
If this takes more than 4 steps, further assessment should take place
(Both TUG and 180 are in NICE falls risk assessment)
Vitamin D supplementation:
Thought to be important because low vit D can be associated with proximal myopathy and therefore falls. A meta-analysis in 2012 showed that supplementation didn’t reduce the overall rate of falls but that it was helpful in certain subgroups.
- Particularly helpful in those with a low vitamin D; fewer people who received vitamin D supplements in this group fell (rel risk 0.70, 0.56-0.87).
- Cochrane review ? helpful for care home residents.
- Useful for bone health in people who fall
Curriculum Mapping:
This episode covers the following areas (n.b not all areas are covered in detail in this single episode):
| Curriculum | Area |
| NHS Knowledge Skills Framework | Suitable to support staff at the following levels:
|
| Foundation Curriculum 2012 | 2.1 Patient as centre of care
6.1 Lifelong learning 6.2 Evidence, guidelines, care protocols and research 10.1 Manages patients with long term conditions 10.2 Supporting patient decision making 10.5 Health promotion, patient education and public health |
| Foundation Curriculum 2016 | 2. Patient as centre of care
4. Self-directed learning 6. Interface with other healthcare professionals 10. Support for patients with long term conditions 16. Demonstrates understanding of the principles of health promotion and illness prevention |
| Core Medical Training | Common competencies:
Symptom based competencies:
System specific competencies:
|
| GPVTS program | Section 2.03 The GP in the Wider Professional Environment
Section 3.01 – Healthy people: promoting health and preventing disease Section 3.05 – Managing older adults
|
| ANP (Draws from KSF) | 7.10 Falls, fractures and other injuries
7.20 Falls, dizziness, syncope 7.26 Immobility and declining mobility 20. Patient as central focus of care 22. Team working and patient safety |
| PA curriculum | 2.3.18 Public health
2.6.3 Patient presentations: Falls |
Feedback
We will add feedback to this as we receive it! The website will have the most up to date version always available: www.thehearingaidpodcasts.org.uk/mdtea
Find Us!
To listen to this episode head to our website, itunes or stitcher.
Give us feedback by emailing us, via twitter or facebook.
Check out our cool infographic A sip of… summarising key points on falls prevention. It’s made for sharing!





1 Response
[…] 2.09: Falls prevention […]