8.10 – Reduced Oral Intake in Dementia
Presented by: Dr Jo Preston, Dr Iain Wilkinson, Dr Alice O’Connor, Chris O’Connor (Consultant Admiral Nurse for Dementia)
Faculty: Dr Wendy Grovesnor
Broadcast Date: 17th December

Social Media
Alice:
Not actually about frailty but made me think about how one’s state of mind can contribute towards frailty (and vice versa), as well as the importance of the language we use in medicine (e.g. frail/ fragile) and what that means to our patients.
Learning Outcomes
Knowledge
- To understand why dementia eventually can lead to a reduced oral intake
- To be able to explain in real terms what is happening (for example, to relatives)
Skills
- To be able to provide practical suggestions as to how to improve oral intake
- To be able to offer suggestions as to how to fortify meals
Attitudes
- To be able to understand that this is part of the process of deterioration in dementia and it may not be possible to ‘fix it’, and that planning for this eventuality is a good idea.
CPD Log
Show Notes
Main Discussion
85% of patients living with advanced dementia in care homes have an eating problem (note NOT a feeding problem – as a colleague of mine says you feed a horse – humans eat – words matter – links to Tom Kitwood’s ideas on personhood.
For an overview of his work look here:
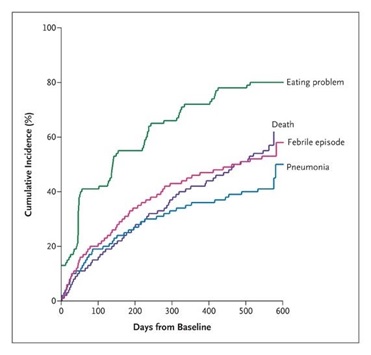
It also occurs sooner and more commonly than infection (febrile episode), pneumonia specifically, and death.
Mitchell et al. The Clinical Course of Advanced Dementia. N Engl J Med 2009; 361:1529-1538
Feeding problems lead onto great stress for relatives, caregivers and, one assumes, the patients themselves.
Men in particular have expressed more concern about nutrition than women when adopting a caregiver’s role, as they were less familiar with household activities, and often have poor cooking skills and poor nutritional knowledge.
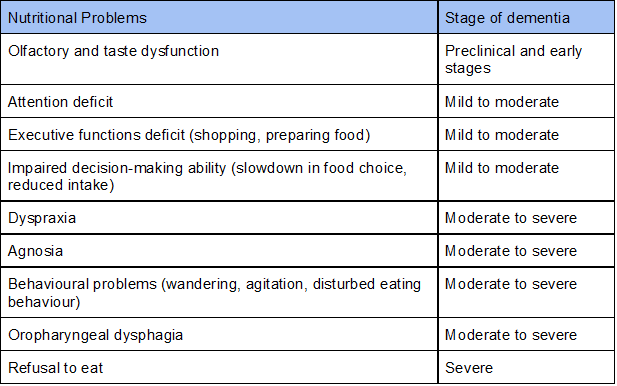
ESPEN guidelines on nutrition in dementia – Clinical Nutrition
In this episode we are not talking about dysphagia or physical problems that may lead to a reduction of oral intake (except maybe an apraxia of chewing that can occur). If you have a patient with a reduced oral intake you should be looking for reversible causes, such as problems with oral health (check out the episode on this), pain in the mouth cavity, or other causes of dysphagia or odynophagia (oesophageal or gastric tumours etc).
There is a good table of these things in the ESPEN guidelines – maybe one day we will talk through them in more detail.
We are also not going to talk about patients who have dementia who have a concurrent delirium or mental health problem that is affecting their oral intake (for example, the patient who is paranoid about care staff or thinks they are being poisoned). Management here should be as per usual to treat the underlying cause.
We are also not going to dwell on the issue of tube feeding. There are a number of review articles out there about the evidence (or lack thereof) regarding this and we can’t cover everything in a short episode!
We know it’s a bit old but this JAMA review is a good starting point.
JAMA, October 13, 1999—Vol 282, No. 14
Weight loss in dementia… how common is it?
There are 850,000 people in the UK with dementia. WHO estimates 5-8% of the population over the age of 60 are affected worldwide.
In advanced dementia, apraxia and attention deficits interfere with self-feeding and dysphagia causes choking or food avoidance.
Eating problems have important health effects such as weight loss, dehydration, poor wound healing and pneumonia.
It’s common – in the CASCADE Study 86% of persons with advanced dementia developed a feeding problem, and onset was associated with 39% mortality at 6 months.
In one study looking at 71 patients with Alzheimer’s Dementia (AD) in institutions, patients were assessed and placed into 4 groups:
1) patients who fed themselves (n = 17, 23.9%),
(2) patients who had to be fed but posed no other eating problem (n = 13,18.3%),
(3) patients who refused food although they were able to swallow it (n = 18, 25.4%), and
(4) patients who choked on liquid and/or solid food, some of whom also refused food (n = 23, 32.4%).
Patients who fed themselves were in a less advanced stage of the disease than those who did not, and their average body weight was equal to the ideal weight.
The remaining three groups (i.e. those with different eating problems) did not differ in mean severity of AD, and their body weights were significantly lower. The mortality rate during the 2 years following the survey was similar in all four groups of patients. Tube feeding was used in only one case.
The mortality rate was also similar in patients whose body weights were 20% or more below the median weight for their age, and in patients whose relative body weight was higher.
The results of this study suggest that eating difficulties occur in a majority of institutionalised AD patients, but can be managed without resorting to tube feeding.
There is an association between stage of dementia and degree of weight loss – but no geographic variation in this.
NERD ALERT
The mechanisms underlying weight loss in dementia are complex, multifactorial and only partly understood
- Some studies have highlighted the role of neurodegenerative processes in specific brain regions, genetic factors and inflammatory processes for nutritional changes in AD.
- Dementia-related brain atrophy may impact regions of the brain involved in appetite regulation and eating behaviour.
- An atrophy of the mesial temporal cortex has been associated with low BMI, suggesting a connection between limbic system damage and low body weight in AD.
- The presence of the apolipoprotein E-e4 allele (APOE), a polymorphism associated with an increased risk of developing AD, has been related to weight loss and a decrease in BMI in women with AD.
- Neuroinflammation is suggested to be of aetiologic importance in AD.
- There are high levels of pro-inflammatory cytokines found in the plasma or cerebrospinal fluid of patients with AD.
- This may also account for dementia-related anorexia and weight loss.
Furthermore, pathological changes in the olfactory system that may occur years before the onset of cognitive decline in AD are thought to contribute to decreased nutritional intake and weight loss .
Studies supporting these findings suggest that olfactory impairment is a pre-clinical marker for dementia and that olfactory evaluations may become a supplementary tool in early detection of dementiA. APOEe4 carriers seem more prone to suffer from impaired olfactory function before the onset of cognitive impairment.
What is happening physiologically?
When you look at patients with AD and those with Vascular Dementia (VD) there is a difference in the pattern of dysfunction of swallowing function.
A Korean study specifically looked at this and found:
“The swallowing disorders of the AD group may result from sensory impairment in relation to dysfunctions in the temporoparietal areas, whereas the swallowing disorders of Vascular Dementia group may primarily be caused by motor impairments due to disruptions in the corticobulbar tract.”
It seems to occur with all forms of dementia but at different stages of the illness.
For example: Dysphagia developed during the late stages of frontotemporal dementia (FTD), but it was seen during the early stage of Alzheimer’s dementia (AD).
Good list of the staging scales here:
https://www.dementiacarecentral.com/aboutdementia/facts/stages/
Limited evidence was available on the usefulness of diagnostic tests, effect of postural changes, modification of fluid and diet consistency, behavioral management and the possible use of medications.
Tips for improving oral intake
Ideas:
Finger food – high calorie content is good!
Food stations around the places – need to be non-perishable items.
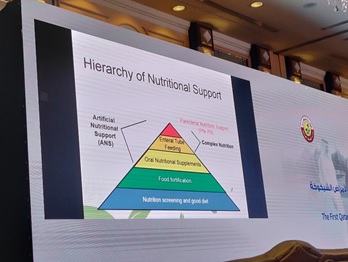
Fortification of food – porridge, build-up drinks etc
Smaller portions – can be problematic with delivered meals
Plate colour – to provide contrast against food colour
Sitting with patients and eating with them
Person centred care e.g. eating in dining room vs alone – what does that person normally do?
Different textures / temperature food
Sweet things first then savoury (If preferred)
What is meal fortification?
A review of 13 trials of the clinical outcomes of oral feeding interventions in patients with dementia found that high calorie supplements and other oral feeding options can help dementia patients with feeding problems to gain weight; they are unlikely to improve other outcomes.
Curriculum Mapping
NHS Knowledge Skills Framework
- Core – Communication level 3
- Core – Quality level 2
- HWB2 – Level 3
- HWB3/4 – Level 2
- HWB5 – level 3
- HWB7 level 2
Foundation Programme
- Section 3.10 – The frail patient
- Section 3.10 – Nutrition
- Section 3.16
Core Medical Training
- Other important presentations – Weight Loss
- Memory loss (progressive)
- Geriatric Medicine
Core Surgical Training
- Dementia
GPVTS
- 3.05 Care of Older Adults
- 3.13 Digestive Health
Geriatric Medicine Specialty Training
- 3.2.3 Presentations of Other Illnesses in Older Persons – Weight loss
- 3.2.2 Common Geriatric Problems (Syndromes) – Dementia
- Core Curriculum
- 29. Diagnosis and Management of Chronic Disease and Disability
- 33, Dementia
Physician Associate Matrix of Conditions
- 1B – Dementia




