6.9 Faecal Incontinence
CPD Log – click here
In this episode we will open up the Pandora’s box that is faecal incontinence (for more info about Pandora’s Box listen the the start of the podcast).
Presented by: Dr Jo Preston, Dr Iain Wilkinson
Guest Faculty: Dr Philippa Christie, Wendy Ness, Wendy Grosvenor
Broadcast Date: 27th November 2018
Here is a pdf of the infographic for you to use
Social Media this Week
Iain:
Greyson Perry – Programme on Rituals – talking about death made by Channel 4
https://www.channel4.com/programmes/grayson-perry-rites-of-passage
Jo:
Systematic review of postural hypotension:
https://academic.oup.com/biomedgerontology/advance-article/doi/10.1093/gerona/gly188/5086075
Phillipa:
BMJ article – blood pressure treatment whilst patients are inpatients.
https://www.bmj.com/content/362/bmj.k3503
Learning Objectives
Knowledge:
To understand the prevalence and problems associated with faecal incontinence
To be able to think through a range of possible diagnoses that are associated with FI
To be able to instigate initial investigation and management for FI in inpatients and outpatients
Skills:
To be able to take a history from a patient with FI
To be able to identify how FI may be affecting your patient
Attitudes:
To understand that FI is a condition associated with a range of potential management options
To understand that FI has a large impact on quality of life and location of care
Show Notes
Click here for a pdf of these to print out.
Definitions:
It is a symptom not a condition in itself.
“Faecal incontinence is the involuntary passage of flatus or faeces through the anal canal.“
The underlying aetiology is often complex with multiple possible contributing factors including:
-
- anorectal structural abnormalities,
-
- neurological disorders,
-
- cognitive or behavioural dysfunction,
-
- stool consistency,
-
- or general disability (particularly age).
- Sometimes no cause can be found.
BMJ Best Practice – Faecal Incontinence in Adults
In Dementia however this is not really enough… as explored in one study based at the university of Hertfordshire:
“a more dementia-focused definition of FI that sees it as an aspect of “toileting difficulties” that may be experienced by people living with dementia. Toileting difficulties are the “voiding of urine or feces either following an unsuccessful effort or with no apparent attempt to use an acceptable facility.” This conceptualization reframes continence in the social and environmental context.
Key Points from Discussion
1. Introduction
This is a common thing… and a common thing we don’t like to think about / talk about.
-
- Depending upon the definition and frequency of faecal incontinence, the prevalence varies from 1% to 10%
- However, when comparable methodologies and definitions are used, studies produce remarkably similar prevalence rates in different community populations (around 8.3% to 8.4% for face-to-face or telephone interviews, and 11.2% to 12.4% for postal surveys)..
BMJ Best Practice – Faecal Incontinence in Adults
-
- Frequency of FI increases with age.
-
- Once UK study (a well constructed postal study) found up to 10% of Men and women >80yrs had at least yearly episodes of FI – 8% for monthly.
-
- 22% had faecal staining on underwear.
- 50% of those with ‘major’ symptoms reported it affecting their quality of life.
That said:
Reported prevalence estimates for fecal incontinence among community-dwelling adults vary widely. A systematic review was undertaken to investigate the studied prevalence of fecal incontinence in the community and explore the heterogeneity of study designs and sources of bias that may explain variability in estimates.
Conclusion:
A consensus definition of fecal incontinence is needed that accounts for alterations in quality of life. Further cross-sectional studies are required that minimize bias in their design and use validated self-administered questionnaires
Macmillan et al. The Prevalence of Fecal Incontinence in Community-Dwelling Adults: A
-
- 1 in 8 adults provide formal care for people. Difficulties in managing continence put an additional strain on this relationship and can lead to carer breakdown. It is the second commonest reason for people to be moved into a care home.
-
- There is a significant link between persons with faecal and urinary incontinence. And an association with greater physical disability.
- Over 50% of people had not discussed the symptom / problem with anyone prior to being asked in one study.
-
- Faecal incontinence disproportionately affects individuals with severe physical and mental disabilities.
-
- Patients living in institutions have an extremely high rate of faecal incontinence.
-
- Poor functional status, impaired cognitive ability, and limited mobility all contribute to incontinence in nursing-home residents, and the rates of incontinence rise with the length of time spent in nursing homes.
- A Canadian study of long-term hospital patients found a prevalence of 46%. Similarly, in a US survey of patients in nursing homes 47% had faecal incontinence.
Similar figures have been found in care homes in USA, Brazil and the UK. It also appears that the longer in a care home the greater the chance of developing FI.
New Zealand: https://www.ncbi.nlm.nih.gov/pubmed/29127713
Brazil: https://www.ncbi.nlm.nih.gov/pubmed/25721982
USA: https://www.ncbi.nlm.nih.gov/pubmed/28407296
Key parts of the history as to how troublesome the symptom is are the frequency of soiling and the volume of leakage of faeces.
Faecal incontinence in care homes is estimated to range from 10% to 50% (ICI 2017)
Rectal carcinoma 20% present with sole symptom of fecal incontinence
Red flag symptoms for bowel cancer
Normal Physiology
Need to understand normal before understanding abnormal.
-
- The GI Tract is amazingly complex. There are more neurons in the GI tract than the spinal cord, and the gut contains sensory neurons specialised to detect chemical, osmotic, thermal and mechanical changes in the gut wall.
- This information is integrated by the CNS via sympathetic and parasympathetic neurons which synapse with the intra-mural neurons and provide the program for the motor neurons. This allows purposeful and coordinated gut programs such as peristalsis and sphincter control.
Pathophysiology of Disease – An introduction to clinical medicine – McPhee 1995
-
- The complex mechanism of continence depends on an interaction of this sphincter function, with that of stool consistency, transit of colonic contents, rectal reservoir function and compliance, anorectal sensation, and pelvic floor anatomy.
-
- Normally, passage of stool or flatus into the rectum allows distension and temporary relaxation of the internal sphincter so that the contents can be sampled by the richly innervated anal transition zone.
-
- Higher centre perception allows further relaxation of the sphincter complex in order to evacuate if socially acceptable. If unacceptable, the external sphincter complex is contracted and the urge to defecate resisted until later.
- Any disruption, dysfunction, or overwhelming of this pathway may result in incontinence.
BMJ Best Practice – Faecal Incontinence in Adults
Causes:
There are essentially 7 aetiological subgroups with patients falling into one or more groups:
Thinking about anatomical then nerve input (control), then stool based factors and finally behaviour
-
- Structural anorectal abnormalities (e.g., sphincter trauma, rectal prolapse) including congenital abnormalities, when symptoms may recur in adult life despite surgical repair
-
- Neurological abnormalities (e.g., multiple sclerosis, stroke, pudendal neuropathy)[7]
-
- Alterations in stool consistency (e.g., infectious diarrhoea, inflammatory bowel disease)
-
- Overflow (e.g., encoparesis, impaction)
-
- Cognitive/behavioural dysfunction (e.g., dementia, learning difficulties)
-
- General disability (e.g., age, acute illness)
- Idiopathic
BMJ Best Practice – Faecal Incontinence in Adults
Management will depend on the cause
Investigations:
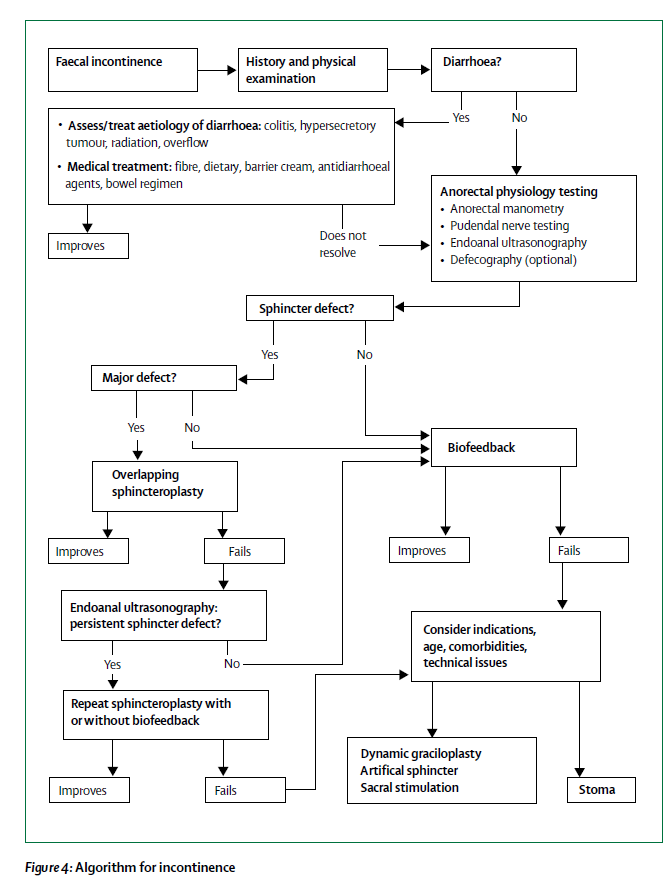
There is an algorithm here (and we will put in the show notes) for the management of FI from an article in the Lancet in 2014. There is a lot of emphasis on quite complex investigations and management that are probably beyond the scope of most people… but it’s worth looking at as:
- a) it shows the importance of treating and diarrhoea first and
- b) it shows the sort of options out there.
Does not really cover overflow / impaction / cancer though – so need to have an index of suspicion about this
From Wendy Ness: Pudendal nerve testing is no longer done and rarely would repeat sphincteroplasty be carried out dynamic graciloplasty on carried out at one centre and rarely would an artificial bowel sphincter be carried out. Could add in Posterior Tibial Nerve Stimulation
Consequence of FI
Thinking about the consequences though also
QOL – as we have seen above this is a large part of the impact and needs active consideration – patients may not vocalise this.
Skin:
Faecal enzyme activity increase/pH increase/Microbes increase
These all lead to increased permeability of the skin > weakened skin > increased risk of pressure damage.
Key points:
-
- Routine skin inspection
-
- Skin cleansing
- Skin protection
Cooper P. Skin Care: managing the skin of the incontinent patient. Wound Essentials Volume 6, 2011
There is good evidence that appropriate diet, fluid intake, and increased mobility help as part of improving FI. The ways in which these strategies are introduced or improved for those residents with dementia should incorporate both the preferences of the person with dementia and consideration of how the activities and routines of the care home support this.
Further research is needed that considers how different care routines and practices can be aligned with interventions to enhance continence care for this population.
Treatment
Diet:
-
- Keep a diary
-
- Contributing foods include prunes, figs, rhubarb, fruit juice and liquorice, and artificial sweeteners can have laxative properties
- Fibre – increase over a few days is recommended. Ispaghula husk/fybogel
Bowel habit:
-
- After meals
-
- Private, comfortable toilets
- Sitting/squatting – This is the sqautty potty video: https://youtu.be/YbYWhdLO43Q
Continence products
Disposable pads
-
- Anal plugs if tolerated
-
- Skin care advice
-
- Odour control products
- Disposable gloves
Emotional/psychological support
- Support groups and coping strategies
Treatment By Aetiology
Loose stool incontinence
-
- Regular antidiarrhoeal agents
-
- Loperamide 1st line – augments anal sphincter, reduces motility and secretions
-
- Codeine if not tolerated
-
- Amitriptylline may reduce rectal motor activity. Long term low dose
- Diphenoxylate/atropine – dose should be reduced over time but can be indefinite
Constipation and overflow
-
- Enemas and suppositories regularly – phosphate and glycerin
-
- Oral laxatives only used if rectal fails
-
- o Lactulose or senna
-
- Oral laxatives only used if rectal fails
-
- Retrograde irrigation – needs dexterity
- Antegrade irrigation – complex, requires appendicostomy (complications include stenosis).
Spinal Cord or neurogenic bowel disorder
-
- Neurological bowel management programme referral
-
- Establish routine – may require manual evacuation or digital anorectal stimulation
-
- Antegrade irrigation
- Sacral nerve stimulation
o Wire through sacral foramen. Can test with temporary wire first.
o Pt does not need to feel stimulation
o Can be reprogrammed over time
- If SNS fails can consider neosphincter but high adverse effects and removal rate.
External Sphincter Deficiency
-
- Pelvic floor exercises
-
- Biofeedback – exercises to improve sensation coordination and strength of floor – using vaginal or anal equipment.
-
- Electrical stimulation
-
- Surgical anterior sphincter repair (less successful if internal sphincter defects, pudendal nn neuropathy or concurrent loose stools
-
- Sacral nn stimulation
- Neosphincter
o Use an alternative mm (eg gracilis) or an artificial cuff device
o Uses a stimulator
Internal Sphincter dysfunction
-
- Pelvic floor exercises
-
- Biofeedback
-
- Electrical stimulation
- Sphincter ‘bulking’ – injecting material into intersphincteric space (including fat, silicon or Teflon!)
Intact Sphincter complex (intact but dysfunctional)/minor tear
-
- Pelvic floor exercises
-
- Biofeedback
-
- SNS
-
- Neosphincter
- TCA – Amitriptylline
Refractory disease
- Stoma
New/emerging treatments
-
- SECCA therapy – temperature controlled radiofrequency remodelling
-
- Posterior tibial nn stimulation – ?efficacy. Can be performed transcutaneously though.
-
- Neosphincter – new types of artificial sphincter including made of magnets
-
- Stem cell injections
-
- New anal plugs and use of vaginal balloons to put pressure on rectum
- Pharmacological therapy – phenylephrine, valproate and clonidine could be useful.
Overflow
Refer back to the episode on constipation. 3.02 – go back and listen to this!
Cognitive/behavioural dysfunction
Regular toileting
Good diet
Be aware when people have had BO and try to time things around this
Gastro-colic reflex use
General disability (e.g., age, acute illness)
Idiopathic
Other References
Ness, W. (2009) Using national guidelines to support the assessment of lower bowel dysfunction. Nursing Times, March 2009, vol./is. 105/12(16-8), 0954-7762 (2009 31 Mar)
Ness, W (2011) Assessing and treating people with bowel dysfunction. Nursing Times, March 2011, vol./is. 107/12(24), 0954-7762 (2011 29 Mar)
Ness, W (2012) Faecal incontinence: causes, assessment and management,Nursing Standard,Volume 26, 42
Ness, W (2013) Management of lower bowel dysfunction, Primary Health Care Volume 23 Number 5
Ness, W (2018) Managing faecal incontinence British Journal of Nursing https://doi.org/10.12968/bjon.2018.27.7.378 Published Online: April 10, 2018
Curriculum Mapping:
This episode covers the following areas (n.b not all areas are covered in detail in this single episode):
| Curriculum | Area | |
| NHS Knowledge Skills Framework | Suitable to support staff at the following levels:
|
|
| Foundation curriculum | 10. Recognises, assesses and manages patients with long term
conditions 11. Obtains history, performs clinical examination, formulates differential diagnosis and management plan 12. Requests relevant investigations and acts upon results |
|
| Higher specialist training – Geriatric Medicine | 3.2.2 Common Geriatric Problems
28. Diagnosis and Management of Acute Illness 29. Diagnosis and Management of Chronic Disease and Disability 34. Continence 48. Continence |
|
| Core Medical Training | The patient as central focus of care
Relationships with patients and communication within a consultation Geriatric Medicine Abdominal Swelling & Constipation |
|
| GPVTS program | Section 2.03 The GP in the Wider Professional Environment
Section 3.05 – Managing older adults
3.13 Digestive Health – Constipation |
|
| Suggested ANP (Draws from KSF) | 7.9 Constipation, diarrhoea, faecal impaction
7.18 Chronic bowel disorders including constipation and incontinence |
|
| PA matrix of conditions | 4. Gastrointestinal | |