6.08 Supporting patients in cancer care
In this episode we focus on how best to support patients who have cancer.
Presented by: Dr Jo Preston, Dr Iain Wilkinson & the
Guest Faculty: Lara Cowley, Shane O’Hanlon
Broadcast Date: 13th November 2018
Here is a .pdf of this sip of MDTea
Social Media
Iain:
Jo:
CPD Log – click here
Learning Objectives
Knowledge:
- To recall the problems experienced by older adults with cancer
- To understand the role of rehabilitation and supportive care in maintaining wellbeing
Skills:
- To recognise when someone may benefit from holistic support
Attitudes:
- To feel confident to talk to someone living with cancer about their options for supportive care
Show Notes
Definitions:
Care given to improve the quality of life of patients who have a serious or life-threatening disease. The goal of supportive care is to prevent or treat as early as possible the symptoms of a disease, side effects caused by treatment of a disease, and psychological, social, and spiritual problems related to a disease or its treatment. Also called comfort care, palliative care, and symptom management.
National Cancer Institute
Cancer rehabilitation is defined as “medical care that should be integrated throughout the oncology care continuum and delivered by trained rehabilitation professionals who have it within their scope of practice to diagnose and treat patients’ physical, psychological and cognitive impairments in an effort to maintain or restore function, reduce symptom burden, maximize independence and improve quality of life in this medically complex population.”
Practical Definition
Any treatment or management plan, regardless of which team is delivering it, which focuses on supporting quality of life, rather than augmenting the primary disease process.
Key Points from Discussion
Diagnosis of cancer can be made in a few different ways
- Following progressive symptoms particular to that cancer e.g. resp, or bowel
- Through non-specific symptom presentations e.g. unintentional weight loss or pain
- Incidentally
Geriatric oncology is expanding as the population ages to recognise the unique needs of older adults and the realisation that routine evaluation, which will assume otherwise reasonably uncomplicated medical, social and cognitive background, is inadequate. It recognises that
- Some form of comprehensive geriatric assessment is required to supplement care
- Predictive models of survival and functional decline exist
- Clinical trials have not met the needs of older patients
More on this in a future episode on the specifics of cancer treatments in older adults.
Also worth bearing in mind 46% of cancer survivors are over 65 (American Cancer Society).
Cancers increase in incidence with advancing age plus by definition survival leads to old age.
Palliative care and oncology
In 2012, the American Society of Clinical Oncology stated that:
Palliative care should be part of standard cancer care for all patients with metastatic disease and/or significant symptom burden.
In 2010, Temel et. al did a study in people with metastatic lung cancer, in which half were over 65. They found that early involvement of palliative care in oncology treatment improved all quality of life measures including:
- Symptom management e.g. pain, nausea
- Quality of life
- Prognostic understanding
- Caregiver outcomes
- Mood
- End of life outcomes
- Survival
- Resource utilization
Palliative care may be considered to extend to survivorship
- Survivorship includes not just patients in remission but where cancer is a chronic disease
- Chronic toxicity of therapy will require various forms of palliation
- Particularly important in older patients
Rehabilitation
Cancer rehabilitation, similar to stroke and orthopedic rehabilitation, utilizes a multidisciplinary approach to assessment and treatment that helps to:
- Address disease-related and treatment-related impairments
- Decrease the number and/or severity of impairments and long-term problems;
- Minimize survivors’ distress and disability.
Patients frequently state their anxieties of becoming a burden to their family and not being able to stay at home. The importance of supporting preferred place of care and preferred place of death can be reinforced with a rehabilitative approach that focuses on function.
Older populations are at increased risk of functional decline and frailty. For this group, small deteriorations in function can have disproportionate impact on capacity for independent living. The loss of function is interwoven with the multiple losses palliative patients experience. The therapeutic relationship developed when working with patients to regain function allows the patient to explore the meanings of these losses and reframe them in a new context.
There is the need to pay attention to nutritional status in relation to function. A reduction in nutritional intake quickly leads to a reduction in functional ability.
Cancer rehabilitation is everyone’s responsibility and should not be confined to specialist services.
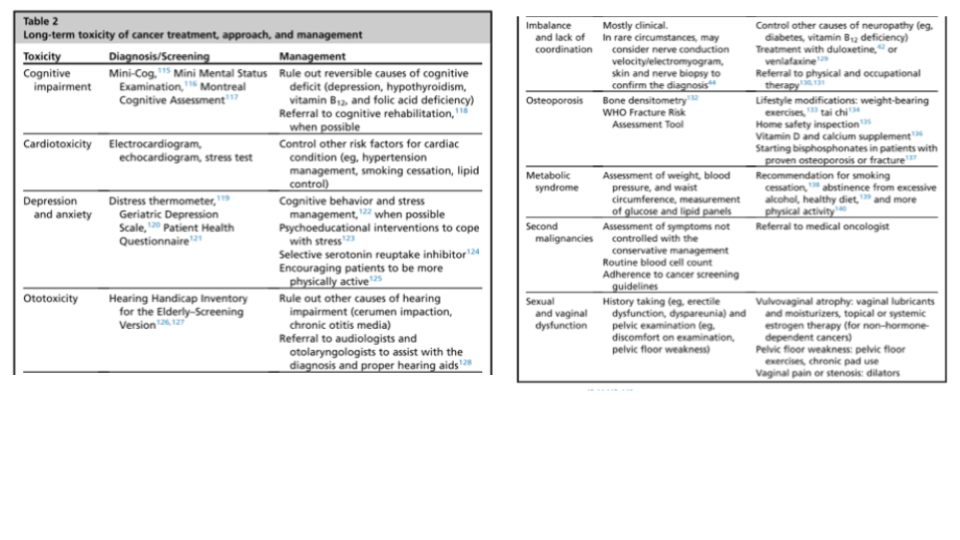
There are specific things related to cancers or the complications of their treatments that need special consideration or monitoring for and these include: (all from CSP ‘So your patient has cancer’)
- Arthralgia: particularly those undergoing hormone treatments (used for cancers that are hormone sensitive or hormone dependent) may suffer with arthralgia which can be distressing and disabling. This can be managed with standard physiotherapy management such as exercise programmes, hydrotherapy, acupuncture and advice.
- Bone metastases: Maintaining mobility is important for many patients, treatment for someone with known bone metastases should be on an individual basis and it’s important to use mobility and strengthening goals where appropriate e.g. avoiding high impact activities. New localised pain may be a sign.
- Breathlessness
- Continence: particularly with pelvic cancers. People who have received pelvic radiotherapy may experience continence issues several years later.
- Fatigue Cancer related fatigue (CRF) is a complex but common symptom for cancer patients which can persist for several years after treatment. Symptoms are multidimensional, but include a persistent lack of energy with sleep and mood both possibly being affected. All physiotherapists should be able to identify CRF and supply basic advice, as well as adapt their treatment depending on severity. Mild to moderate intensity exercise can help. OTs can help with energy conservation training, translating to practical strategies to manage fatigue for resumption of roles and routines
- Lymphoedema: as a result of lymph node infiltration or surgery. Unlike ‘usual’ lymphoedema, this can often affect upper limbs in those who have had breast cancer in particular and OT may be able to help with strategies associated with, pain and reduced ROM for example.
- Nerve damage: Peripheral neuropathy is a common side effect of chemotherapy treatment which is often temporary but in some instances may be permanent. Surgery for cancer treatment may also lead to nerve impairment.
- Osteoporosis: Some cancer patients, for example those with breast, gynaecological or prostate cancer, are at increased risk of developing osteoporosis due to the treatment they have received.
- Pain: Musculoskeletal (MSK) pain can occur as a result of cancer or its treatment. This MSK pain can be assessed in the same way as other MSK problems and often responds well to physiotherapy, particularly in conjunction with input from other members of the multidisciplinary team (MDT).
- Psychological issues 80% of patients have anxiety and depression following a cancer diagnosis but often physiotherapists can help a number of these patients by addressing their symptoms and maximising daily function.
- Cancer-related cognitive impairment (CRCI) presents as difficulties related to memory, attention, information-processing speed, and organization, and can affect all age groups. For example, women with breast CRCI report mild cognitive decline impacting their ability to function, making previously easy activities more difficult and causing distressing loss of independence in family life roles
CSP: So your patient has cancer? A guide for physiotherapists not specialising in cancer
Occupational therapy for adults with cancer: why it matters. Pergolotti et. al, Oncology 2016.
There is evidence that the diagnosis of cancer provides a “teachable moment”, when discussions about physical activity are likely to be well received by the patient. Many people need support to change to a healthier lifestyle, especially with physical activity as they may be fatigued, lack confidence and are anxious about causing damage. Physiotherapists are in a unique position to support people to become more active.
Occupational therapy perspective:
Adults with cancer are at a higher risk for functional limitations, poorer QOL, and falling. Poor QOL and functional limitations are associated with decreased ability to complete full treatment, increased risk of receiving a less intense treatment regimen, increased risk for chemotherapy toxicity, and, in turn, decreased survival. In patients with metastatic disease, one in five adults with cancer reported cognitive difficulties and 66% reported functional deficits. Adults stated they had difficulty with bending, stooping, lifting, and getting out of bed and they needed help with ADLs often.
Occupational therapy for adults with cancer: why it matters. Pergolotti et. al, Oncology 2016.
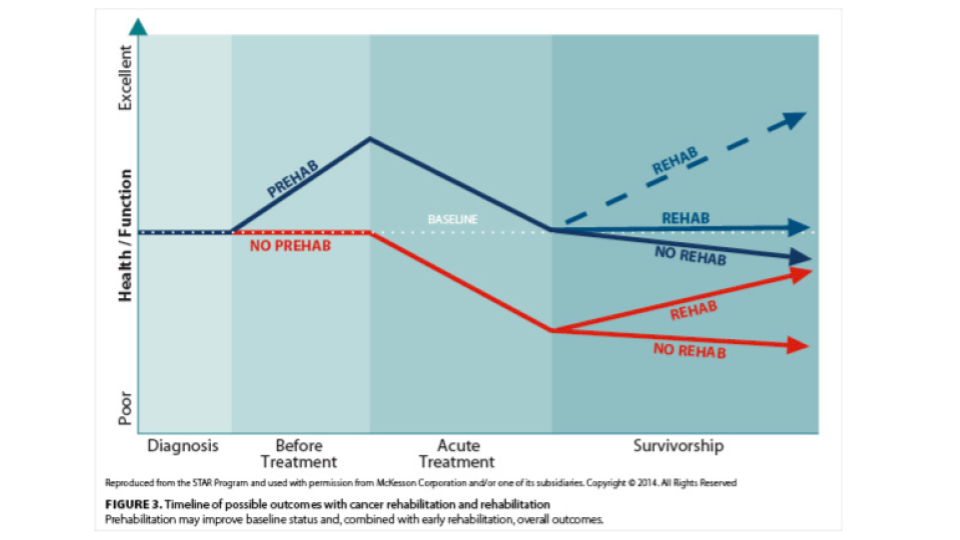
Prehabilitation is medical care that may help newly diagnosed cancer survivors prepare for upcoming treatments and either prevent or reduce the likelihood of long-term problems.
Prehab focuses on effort to reduce physical impairments, functional disability, pain and emotional distress. This, in turn, may reduce direct and indirect healthcare costs and ultimately improve health-related quality of life.
Improve cardiovascular, pulmonary, and/or musculoskeletal function.
- Improve balance and reduce the risk of falls.
- Reduce anxiety and improve coping with specific cognitive behavioral strategies.
- Improve quality of sleep with sleep hygiene education.
- Optimize surgical outcomes with smoking cessation interventions.
- Optimize diet with nutrition counseling.
- Begin preoperative pelvic floor muscle strengthening to improve continence outcomes.
- Begin pretreatment swallowing exercises to improve swallowing outcomes.
- Implement home safety strategies to avoid falls.
- Facilitate return to work with adaptive equipment.
At all stages, opportunities should be taken to assess for care needs both of the individual and any carers, as we’ve discussed in previous episodes.
Long term toxicities of cancer treatment in older patients. Shahrokni et. al 2016
Curriculum Mapping
| Curriculum | Area | |
| NHS Knowledge Skills Framework | Suitable to support staff at the following levels:
| |
| Foundation curriculum | Section
2 6 7 10 | Title
Delivers patient centred care and maintains trust Communicates clearly in a variety of settings Works effectively as a team member Recognises, assesses and manages patients with long term conditions |
| Core Medical Training | Patient as central focus of care
Relationships with patients and communication within a consultation Management of Patients Requiring Palliative and End of Life Care | |
| PA matrix of conditions | A number of cancers are mentioned specifically – Breast, oral and endometrial | |
| GPVTS program | Section 2.01 The GP Consultation in Practice
Section 3.05 – Managing older adults
| |
| ANP (Draws from KSF) | Managing Long-Term Conditions and Promoting Patient Self Care | |
| Geriatric Medicine Training Curriculum | 6. Patient as the Central Focus of Care
11. Managing Long Term Conditions and Promoting Patient Self Care 12. Relationships with Patients and Communication within a Consultation. 29. Diagnosis and Management of Chronic Disease and Disability |





1 Response
[…] Podcast: Supporting patients in cancer care, […]