9.07 Teamworking
Presented by: Iain Wilkinson, Jo Preston, Sophie Norman.
Additional Guests: Julian Stodd (Author and Founder of Sea Salt Learning)
Broadcast date: 24th November 2020

Social Media
Iain: @parthaskar retweeted this beautiful video of former Prima Ballerina Marta Gonzalez who lives with dementia listening to music from Tchaikovsky’s Swan Lake
Jo: @age_uk report on the impact of COID-19 on older persons, via Cate Bailey @_parapraxis_
Learning Outcomes
Knowledge
- How teams form and what binds them together
- To be able to understand situations that put teams unders strain / stress
- To introduce the ideas of social currency and social leadership
Skills
- To be able to identify problems in teams and have some skills to address them
- To be able to build a team and know the unwritten rules about this
Attitudes
- To understand that all team members want the best outcomes for patients
CPD Log
Show Notes
Introduction
- In the past there was the ‘good’ doctor who knew everything about their patient, they knew all the blood test results, investigations and procedures the patient had had. They saw patients in the outpatient department, when they were admitted to hospital, and at home. They knew their wife, husband, parents and children….
- Nothing was hidden from the ‘good’ doctor.
- Nursing care, when it was needed, might be provided by family members (and in some countries still is).
- The concept of a coordinated multi-professional team giving personalised patient centred therapy was a distant spec on the horizon….
- Now things are different… these doctors don’t exist anymore…
- there are more patients than ever before,
- a higher workload and
- many many more investigations, procedures and staff working with patients.
- More knowledge leads to more knowledge.
Doctors, nurses, therapists cannot keep up with all this on their own. We need to work together and healthcare is now a team sport…
- But are we really taught about how to play in the team?
- What position are we in?
Formal definition
To ‘team’: (verb) come together as a team to achieve a common goal.
“Team-based health care is the provision of health services to individuals, families, and/or their communities by at least two health providers who work collaboratively with patients and their caregivers—to the extent preferred by each patient— to accomplish shared goals within and across settings to achieve coordinated, high-quality care.”
Naylor MD, Coburn KD, Kurtzman ET, et al. 2010
in:
Mitchell, P., M. Wynia, R. Golden, B. McNellis, S. Okun, C.E. Webb, V. Rohrbach, and I. Von Kohorn. 2012. Core principles & values of effective team-based health care. Discussion Paper, Institute of Medicine, Washington, DC. www.iom.edu/tbchttps://nam.edu/wp-content/uploads/2015/06/VSRT-Team-Based-Care-Principles-Values.pdf
Main Discussion
Practical definition
Practically we are in lots of ‘teams’
- Teams in health are heterogenous
- can be large or small, centralized or dispersed, virtual (increasingly over recent months) or face-to-face
- Tasks assigned to a team can be focused and brief or broad and lengthy.
- Different patient types
- Different settings
- This makes defining optimal team-based health care a challenge – and much of the research is only in teams based in the acute settings
- Regardless of this, effective teams throughout health care are guided by basic principles that can be measured, compared, learned, and replicated.
We may have different roles within each team and there may / will be different ‘rules’ for each team.
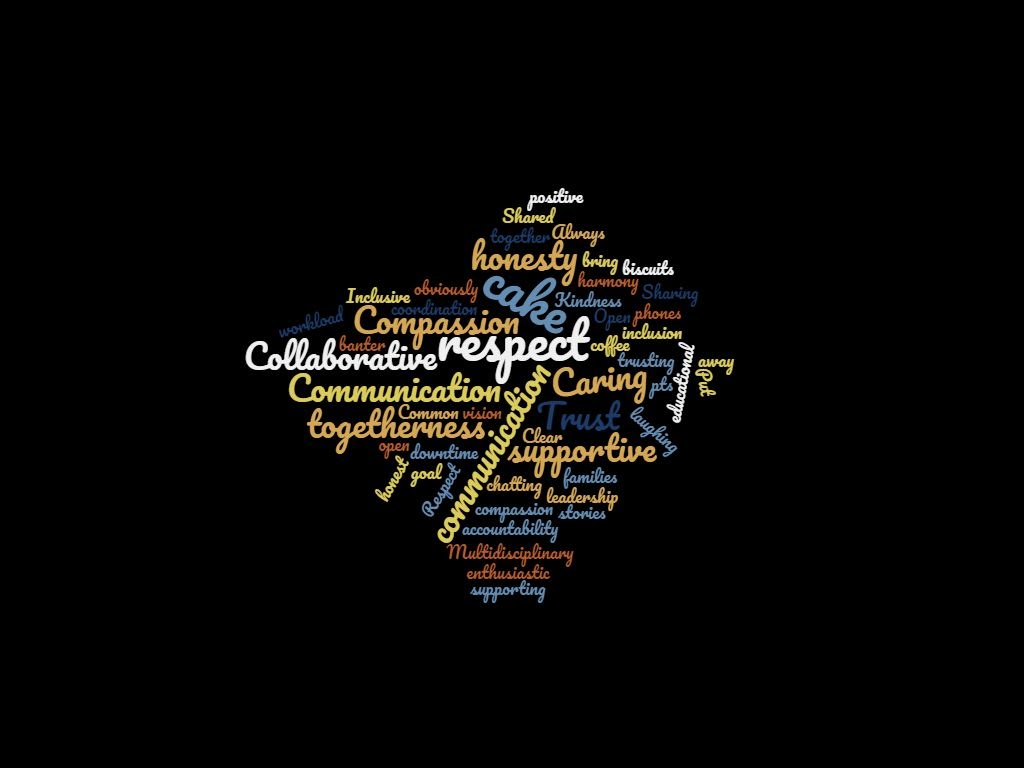
These were the responses we received to a call on twitter for three words to describe what a good team means to people (see #MDTeaclub on twitter);
- Trust, respect, togetherness
- Inclusive, open and honest
- Common goal. Collaborative. Caring
- Compassion, leadership, banter.
- Collaborative, enthusiastic, supportive
- Caring, laughing and respect!
- Put phones away
- Sharing (workload, cake, stories), supporting (each other, pts, families) positive
- Always bring biscuits
- Shared vision, accountability and cake (obviously!)
- Kindness, compassion and togetherness
- coffee, cake, chatting. – downtime together
- Trust, inclusion, honesty
- Communication, honesty and respect
- Communication, harmony, and support.
- Multidisciplinary, Clear communication
- Open, trusting, educational
- Respect each other
- Compassion, communication, coordination
Word Cloud of responses to our #MDTeaclub question:
5 Principles of Team-Based Health Care
- Shared goals: The team—including the patient and, where appropriate, family members or other support persons—works to establish shared goals that reflect patient and family priorities.
- Clear roles: There are clear expectations for each team member’s functions, responsibilities, and accountabilities. This idea might be argued against in some cases, as in the example of the MDT where blurring of roles is encouraged and helpful.
- Mutual trust: Team members earn each others’ trust, creating strong norms of reciprocity and greater opportunities for shared achievement.
- Effective communication: The team prioritizes and continuously refines its communication skills.
- Measurable processes and outcomes: The team agrees on and implements reliable and timely feedback.
https://nam.edu/wp-content/uploads/2015/06/VSRT-Team-Based-Care-Principles-Values.pdf
Reflecting on team-working in the health and social care environments with Julian Stodd, author, researcher and founder of Sea Salt learning
- We are describing on twitter how we LIKE to experience teams – we like to like people, we like to be together.
- The theme of having coffee and cake together as teams comes up surprisingly often! This can be seen in Julian’s ‘Landscape of Trust’ research – carried out 2018-2019 (over 30 different organisations).
- However, you could contort and break the definitions that have been suggested on twitter and that we have discussed above and still have an effective and functioning team – for example;
- A team might function with there are no clear roles
- A team might be chaotic
- There might be trust of each other within a team, but a unifying mistrust in others
- Communication might be largely opportunistic and done using diverse technologies.
Stodd, J. (2018). The Trust Guidebook. (Sea Salt Publishing)
Trust and ‘tribes’
Trust – this is not a logical entity.
- Trust is not evenly distributed throughout an organisation.
- As systems and organisations become more formal, and hierarchy is created, trust collapses down. It becomes easier to frame this in terms of ‘tribes’
- These tribes are trust-bonded structures which sit within communities and teams
- Trust, like leadership, is something we cannot buy/expect or demand it from others. We can only earn it.
So what is the difference between these tribes and communities/organisations themselves?
- Tribes don’t necessarily relate to the structure of communities/organisations in which you exist
- We all belong to lots of different tribes – ie we exist within lots of different groups of people who trust each other
- We may present different versions of ourselves in these different spaces
We also belong to many different communities
- NHS contingent research (of 5000 people) in 2018 – found on average, people identified 15 different communities in which they belonged.
- A community is ‘meta-tribe’ – and we may not have an equally strong relationship with everyone in that community
Julian Stodd (2020) ‘Tribes, Communities and Society: A Reflection on Taxonomy’. Julianstodd.wordpress.com. November 2017. Available at: https://julianstodd.wordpress.com/2017/11/03/tribes-communities-and-society-a-reflection-on-taxonomy/ (Accessed: 23/11/2020)
Julian Stodd (2020) ’The Scale of Social Systems: Tribes, and Tribes of Tribes’. Julianstodd.wordpress.com. 2017. Available at: https://julianstodd.wordpress.com/2017/10/18/the-scale-of-social-systems-tribes-and-tribes-of-tribes/amp/ (Accessed: 23/11/2020)
Stodd, J. (2019). The Community Builder Guidebook. (Sea Salt Publishing)
As an individual progresses upwards within an organisation, we find they will hold more of themselves back.
- In a more senior role, there is a permanence of action and formality of consequence not seen lower down the taxonomy of an organisation
- Things that are effective in a trust-bonded group because of things like common vocabulary, accepted rule-bending etc are not possible in a more senior position.
- Within trust-bonded groups, we can be uncertain and we can learn and prototype new behaviours without great concern over the consequences in a way that we cannot in a more formal, senior role.
The patient within the healthcare team
‘Meta-effects’ emerge out of complex interactions (ie within large organisations such as the NHS)
- Thousands of people are formally held within their disciplines and use formally learnt knowledge,
- Healthcare has to be formally organised to achieve replicability at scale
- This structure gives us a measurable outcome (visible to us as members of the organisation)
- A patient or relative’s experiences of the organisation does not sit within that structure in the same way
- Concepts and goals are different from the healthcare teams perspective compared to that of the patient and relative.
- Excellence within the system often happens outside the formalised structures and roles – and is often down to an individual
Learning how ‘to team’
Within health and social care, we generally have all been through broadly similar foundational training
- We have to develop the art of taking the formal knowledge we have learnt and blend it with the experience of others and the environment around us
Research into ‘communities of practice’ suggests we learn from the people who are around us – i.e. from the wider team. However, generally we are taught in our single disciplines.
Wenger, E. A Social Theory of Learning. Illeris K., ed.. Contemporary Theories of Learning. Oxford:Routledge (2009) pg 209-218.
We also need to be aware of teams that are ‘effective’ and ‘functioning well’ with regards to certain measurable outcomes, which may actually be resulting in additional negative outcomes. For example, a well bonded team might harbour malpractice with the coherent and conforming behaviour of the team silencing dissenting voices.
- How can we engender speaking up as the leaders or team members?
- Tuckman’s model:
- We are often dropped into teams and the members of each team may change quite regularly with rotational jobs.
- Results in frequent cycles for MDTs of:
- Forming
- Storming (turbulence when roles are formed)
- Norming (things going okay)
- Performing (productive)
https://www.mindtools.com/pages/article/newLDR_86.htm
- Being aware that this process is happening can be helpful as we can identify stages and enable productive discussion.
- Having an awareness of the team around you is important
- This is shown practically with the ‘heads up’ experiment/example
(https://youtu.be/vJG698U2Mvo)
- Be aware of praising teams/team members and those around you who these positive stories may disempower or exclude.
- Use issues within teams and opportunities to grow and develop the team- take people for coffee and cake!
- Coffee and cake might seem pointless when looking at outcomes and purpose….but you can’t have purposefulness without pointlessness
- With the ‘pointless’ coffee and cake, you’re laying foundations for strength within the teams.
Forming tribes and teams
- We have a ‘primary cultural alignment’ with the first team we work with/first take responsibility with.
- These bonds may remain for some time.
- We don’t have the ability to continue to make such enduring bonds with team members – though we can give the impression of doing so.
- We form tribes (our ‘primary cultural alignment’) quite fast
- There is also an idea of a ‘secondary cultural alignment’ within organisations
- This is akin to having geopolitical power.
- It involves finding a voice within the organisation to facilitate an individual to achieve influence.
- It is based on experience – ie an individual cannot be given this power without earning it.
- Most people never get to a position of secondary cultural alignment, as regularly changing roles mean we stick with primary cultural alignment and the relationships that sit outside the job roles.
- We should engender a willingness to give shelter and power to others within the team (when we have more senior roles)
- We must recognise that we all have the ability to effect change within teams.
Stodd, J. (2019). Finding your campfire. A Remote Working Survival guide. (Sea Salt Publishing)
Available at: https://seasaltlearning.com/finding-your-campfire-a-remote-working-survival-guide/. (Accessed on: 23/11/2020)
Curriculum Mapping
NHS Knowledge Skills Framework
- Core
- Communication – Level 3
- Personal and people development – Level 2
- Service Improvement – Level 2-3
- G6 People management – Level 2-3
- G2 Development and innovation Level 2
Foundation Programme
- GMC domains: Communication, partnership and teamwork
- 1. Acts professionally – Personal Organisation
- 4. Keeps practice up to date through learning and teaching
- SECTION 2: Communication, team-working and leadership
Internal Medical Training
- GMC domains: Communication, partnership and teamwork
- Generic CIP: 3. Communicates effectively and is able to share decision making, while maintaining appropriate situational awareness, professional behaviour and professional judgement
- Speciality CIP. 6. Managing a multi-disciplinary team including effective discharge planning
Core Surgical Training
- Module 4- The assessment and management of the surgical patient – Team working and planning
GPVTS
- GMC domains: Communication, partnership and teamwork
- Core Competence: Working with colleagues and in teams
- 2.01 The GP Consultation in Practice
- 2.02 Patient Safety and Quality of Care
- 2.03 The GP in the Wider Professional Environment
- 3.05 Care of Older Adults
Geriatric Medicine Specialty Training
- GMC domains: Communication, partnership and teamwork
- 3.1 To work effectively within a multidisciplinary team to promote the optimal recovery of patients and plan their safe transfer of care between all relevant settings.
- 7. Prioritisation of patient safety in clinical practice – Encourage feedback from all members of the team on safety issues
- 8. Team Working and Patient Safety
- 15. Communication with Colleagues and Cooperation – The features of good team dynamics




