11.7 A Day in the Life of an Occupational Therapist
Presented by: Iain Wilkinson, Stephen Collins, Georgie Gill
Special Guests: Bex Allen, Rebecca Griffith, Alanna Millar, Oran Quinn, Katie Taylor, Suzanne Taylor, Louise Tolley, Paul Wilkinson
Broadcast date: 5th April 2022
Learning Outcomes
Knowledge:
- To know the role played by OT’s and see the pivotal role they play in helping patients continue to perform meaningful and important activities in later life
- To understand the difference between the unique roles played by physios and OT’s
- To recognise the highly specialised problem-solving skills which OT’s possess and make use of every day
- To understand the meaning of everyday terms and concepts used by OT’s such as “grading” and “occupation”.
Skills:
- To learn how to listen to patients, like OT’s do, in order to find out what it is that the patient wants and to remember to keep them at the centre of all the goals we set
- To become more creative, like OT’s, in coming up with ways to help patients rehab and prepare for home life even while they’re undergoing treatment as an inpatient
Attitudes:
- To help all other healthcare staff in the hospital setting understand the value that OT’s can bring to the care of older patients.
Social Media this week
Georgie: Natalie Sharman- Traffic light mouthcare trial, happening at Barnet hospital. Colour-coded list of equipment for hospital patients.
Iain: World Parkinson’s Day – 11th April – Stand up for Parkinson’s challenge. Parkinson’s Disease is the 2nd most common neurodegenerative condition in the UK, so it’s really important for us to have good awareness of it, and to make sure people get the right meds at the right time.
Key Learning Points about OT's
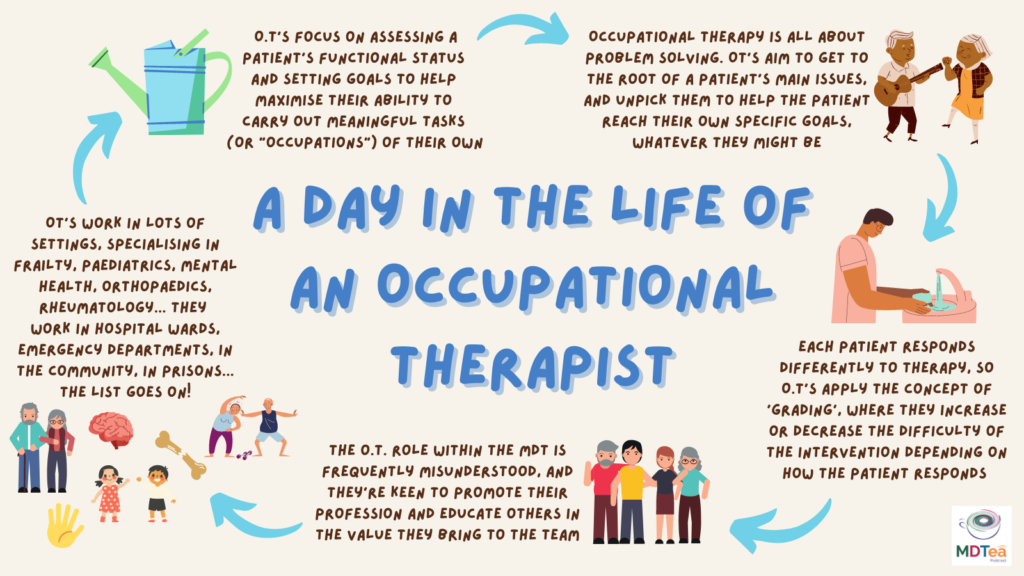
1) The role of an OT focuses on assessing a patient’s functional status and setting goals to help maximise their ability to carry out meaningful tasks (or “occupations”) of their own.
2) OT’s feel that their role and their place in the MDT is frequently misunderstood, and they are keen to promote their profession and educate others in the value they bring to the team.
3) OT’s find that each patient responds differently to therapy, and so they apply the concept of ‘grading’ when reviewing patients on the ward, where they increase or decrease the difficulty of the intervention depending on how the patient is responding to it.
4) Occupational therapy is all about problem solving, with nearly every OT we spoke to for this episode highlighting this as the most important skill to possess for the job. OT’s try and get to the root of a patient’s main issue, and unpick it to help the patient reach their ultimate goal, whatever that might be.
5) OT’s can work in a range of settings in hospital, both on inpatient wards and in the Emergency Department as part of a front door frailty service. In each of these environments they look for ways to make changes (big and small) to help patient’s live their life in a more independent and enjoyable way.
Some facts and figures about OT's
The primary goal of occupational therapy is to enable people to participate in the activities of everyday life. Occupational therapists achieve this outcome by working with people and communities to enhance their ability to engage in the occupations they want to, need to, or are expected to do, or by modifying the occupation or the environment to better support their occupational engagement. (WFOT 2012).
Places of employment for OT’s may include hospitals, clinics, day and rehabilitation centres, home care programmes, special schools, industry and private enterprise.
OT originated as a profession over 100 years ago, after the founding meeting for the National Society for the Promotion of Occupational Therapy in New York on March 15th 1917.
There are approximately 47,300 occupational therapists working in the UK today (Statista, 2021).
Many older people receive occupational therapy as a way to help perform “occupations” or activities of daily living (ADLs) – including everything from bathing and toileting to getting dressed in the morning.
Some of the main ways that OT’s help older patients are by helping them overcome daily challenges, modifying their homes, improving their mental wellbeing, and promoting independence.
Occupational therapy helps older people stay at home, and reduces the number of times they require admission to hospital (Age UK, 2016).
All occupational therapy helps with activities that are meaningful to the patient, so a good OT goal should always be functional and patient-centred.
Useful Definitions
Occupation= In occupational therapy, occupations refer to the everyday activities that people do as individuals, in families and with communities to occupy time and bring meaning and purpose to their lives. Occupations include things people need to, want to and are expected to do. These can be daily tasks like washing and dressing, but can also be pleasurable acitivities like reading and brushing their hair.
Grading= Grading OT interventions refers to increasing or decreasing the difficulty of the intervention you’ve provided based on how your patient is responding to it. If the activity is too easy you would grade it up to make it a greater challenge, or on the other hand you would simplify it if they are finding it too challenging.
Activities of daily living (ADL’s)= activities which involve taking care of one’s own body and are fundamental to living. These activities include dressing, bathing/showering, toileting, eating/feeding, functional mobility, and personal hygiene.

How would the OT's help with Jean?
Get some background on how Jean has been managing with basic daily activities like washing, dressing and toileting on the ward so far.
Introduce themselves, and talk to Jean as a way of establishing whether she has capacity to make informed decisions on her own discharge when the time comes.
Phone Jean’s family to gain a full collateral history (due to Jean’s history of dementia) and find out what Jean is normally able to do at home independently, and also to hear what things Jean enjoys doing and the things that bring meaning to her everyday life.
Make initial plans for the goals that they might aim for as part of Jean’s rehab.
May decide to do a kitchen or bathroom assessment on the ward, to see how she physically copes doing these tasks without assistance.
Consider whether or not Jean would benefit from any new home adaptations, such as handrails, stairlifts, dementia clocks, pendant alarms, perching stools etc – to improve both her safety and her quality of life.
Daily reviews of how Jean is progressing towards her agreed goals, and ‘grading’ the difficulty of tasks as appropriate as she improves.
Refer on to other community services prior to Jean’s discharge, such as a Frailty service or a Community Dementia service.
Also refer to their Community OT colleagues, to arrange a home visit in the near future to monitor how Jean is adapting to being back at home again, and to see if she is living the home life she wants to.
What did we learn from each OT we spoke to?
Louise– her motto is that “life is worth living”, and she enjoys working with patients who have complex needs to achieve goals that make their life worth living again.
Katie– explained that ‘occupations’ in OT involve not only the essential daily tasks that a patient needs to do (like washing and dressing) but also “meaningful and enjoyable activities” like reading or walking to the shop.
Paul– talked about the rewarding nature of his job. He often finds that the smallest things (like a handrail or a commode) can make big, life-changing differences to how a person manages at home.
Rebecca– described the importance of rapport with an older patient, and how this leads to trust. Then the OT and patient can cooperate to set and work towards goals.
Oran– taught us that “occupations” can vary widely. One person’s desire may be that they want to be able to dress themselves at home, while others might be to walk their dog. OT’s break that goal down, see where the person is struggling, and then try and promote independence.
Alanna– said a big challenge for her at work is when other healthcare staff don’t understand the role of OT’s. She thinks that it’s important for us to work hard to educate staff so that they understand the role more.
Suzanne– said that everyone rehabs at different rates. OT’s try and work with a patient’s goals, but sometimes those goals need adjusted and you have to be creative as the OT with that patient.
Bex– reminded us that “medically fit for discharge” does not mean “therapy fit”. She touched on what it is like to work with the constant pressure to discharge patients which can often unfortunately hamper OT work.
#MDTeaser
Curriculum Mapping
NHS Key Skills Framework
Core
Develop and maintain communication with people on complex matters, issues and ideas and/or in complex situations
Health and Wellbeing
Assess physiological and/or psychological functioning and develop, monitor and review related treatment plans.
Plan, deliver and evaluate interventions and/or treatments
Design, produce and adapt equipment and devices
Prepare and supply specialised products
Foundation Curriculum
Year One and Year Two
1.2 Patient centred care
Works with patients and colleagues to develop individual care plans
2.6 Communicates clearly in a variety of settings
Makes clear, concise and timely written and oral referrals to other healthcare professionals within the hospital
2.7 Works effectively as a team member
Acts as a member of the multidisciplinary professional team by supporting, respecting and being receptive to the views of other healthcare professionals
Works effectively with others towards a common goal e.g. accepts instructions and allocation of tasks from seniors at handovers and multidisciplinary team meetings
3.10 Recognises, assesses and manages patients with long-term conditions
Formulates individual patient management plan based on assessment of frailty as well as clinical need
GP Training Curriculum
Communication and consultation
Have appropriate communication skills for counselling, teaching and treating patients, their families and carers, and recognising the difficulties of communicating with older patients
Making decisions
Recognise the importance of a problem-based approach, taking in the ‘big picture’, rather than a disease-based approach to the care of older people, who often have complex physical, psychological and social problems
Clinical management
Understand the physical factors – particularly diet, exercise, ambient temperature and sleep – that disproportionately affect the health of older people
Know how to access support services for older patients, e.g. podiatry, visual and hearing aids, immobility and walking aids, meals on wheels, home care services
Know the different forms of day-care and residential accommodation available and be able to advise patients about them
Ensure that the provision of care promotes the patient’s sense of identity and personal dignity, and that the patient is not discriminated against as a result of their age
Core Medical Trainee
- Common competencies:
Managing patient conditions and promoting patient self-care
Outline the concept of quality of life and how it can be measured
- Geriatric medicine competencies:
Understand the factors which influence health – psychological, biological, social, cultural and economic especially work and poverty
Internal Medicine Training Curriculum
Generic CiP3:
Communicates effectively and is able to share decision making, while maintaining appropriate situational awareness, professional behaviour and professional judgement
Geriatrics and Higher Specialty Training Curriculum
- Comprehensive geriatric assessment
Recognise that good health includes both physical and mental wellbeing and social, sexual and spiritual aspects
- Rehabilitation and Multidisciplinary Team Working
Principles of rehabilitation and comprehensive assessment
Roles and expertise of different members of interdisciplinary team
Reference List
The World Federation of Occupational Therapists (WFOT), ‘About Occupational Therapy’ = https://wfot.org/about/about-occupational-therapy
Prestige Nursing, ‘The Benefits of Occupational Therapy for Seniors’= https://www.prestige-nursing.co.uk/activities/occupational-therapy-activities-for-the-elderly/
Age UK, Occupational therapy helps older people stay at home, July 2016= https://www.ageukmobility.co.uk/mobility-news/article/occupational-therapy-helps-older-people-stay-at-home
OT Centennial, ‘Important Events’= http://www.otcentennial.org/100-events/1917
Occupational Therapy Toolkit, ’10 Facts about OT’= https://www.ottoolkit.com/blog/10-facts-about-ot/
Royal College of Occupational Therapists (RCOT), ‘Occupational Therapy in the Prevention and Management of Falls in Adults’= https://www.rcot.co.uk/practice-resources/rcot-practice-guidelines/falls
My OT Spot, ‘Grading Occupational Therapy Interventions’= https://www.myotspot.com/grading-ot-interventions/
Statista, ‘Annual number of occupational therapists in the United Kingdom (UK) from 2010 to 2021’= https://www.statista.com/statistics/318909/numbers-of-occupational-therapists-in-the-uk/
BRAINS Potential, ‘Common Occupational Therapy Terms You Should Know’= https://brainspotential.com/common-occupational-therapy-terms-you-should-know/
