6.02 Postural Hypotension
Postural Hypotension
This episode and the next look at two opposite sides of a the common problem of blood pressure.
Presentedby: Dr Jo Preston & Dr Iain Wilkinson
Core Faculty: Wendy Grosvenor, Edda Hensler, SJ Ryan
Show notes for download are here
Click here to download and share this infographic
Social Media This Week
Iain:
Interesting study shows major disruptions in sleep when patients are hospitalized. Average patient loses 83 minutes of sleep per night compared to home. Not a good thing in patients who are trying to recover from acute illness #geriatrics #hpm https://t.co/SpeDOWeEdw
— Ken Covinsky (@geri_doc) July 16, 2018
Jo:
Lovely article about people with dementia reviewing dementia friendly tableware https://t.co/5Tyj4EJlLQ
— Thea (@DrTheodoraJones) July 20, 2018
The Gallery
Enlightenment After Dark, a Radio 4 show.
(This particular episode called bodies.)
Show Notes
Click here format PDF of the show notes
Learning Outcomes
Knowledge:
- To understand the mechanisms behind postural hypotension
- To be able to recall common causes
Skills:
- To be able to take an accurate lying and standing blood pressure
- To recognise when instability and pre syncope may be due to postural hypotension
Attitudes:
- To appreciate the impact of postural hypotension on an individual
- To recognise the role for MDT approach to managing this condition
Definitions:
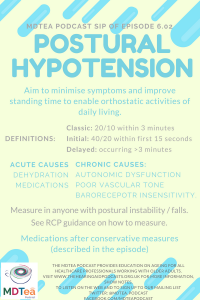
Postural hypotension is defined as a drop in blood pressure from lying to standing of 20/10 within 3 minutes of standing.
20/10 came from quite a small initial study which probably wasn’t sufficiently powered to have an accurate prediction but this number has been replicated many times in other studies so stands as a working figure.
Practical Definition:
Any postural symptoms clearly related to standing.
Classic definition: 20/10 within first 3 minutes of standing (but first 30 seconds most likely).
Initial: 40/20 in first 15 seconds (need to be doing beat to beat recording to catch this).
In Hypertensives: 30 systolic as variability higher in this group.
Delayed: no agreed definition but occuring > 3 minutes
New Horizons in Orthostatic Hypotension, Frith & Parry, Age & Ageing 2017
The practical goal is to improve standing BP so as to minimize symptoms and to improve standing time in order to be able to undertake orthostatic activities of daily living, without excessive supine hypertension.
Orthostatic Hypotension: Mechanisms, Causes, Management. Low & Tomalia. J Clin Neurol. 2015
Key Points from Discussion
Introduction
Common cause of postural instability, falls and reduced confidence.
Links to dizziness episode from series 1.
Reminder of it being less important to use the words that people use to describe their symptoms in older adults so may use terms interchangeably: dizziness, lightheadedness, vertigo. Young people more likely to say spinning.
Syncope is transient global cerebral hypoperfusion.
- Transient, self limiting loss of consciousness
- Rapid onset
- Recovery is spontaneous, complete and usually prompt.
Generally the brain is very good at maintaining a stable blood flow except at the extremes of blood pressure i.e. very high or very low. This can change as we age and this regulation of a steady blood pressure is less well controlled, leading to the brain being more vulnerable to changes in body blood pressure.
Syncopal disorders can be varied in their causes, so an important first step is to make sure that this person is seen by a clinician who is able to determine whether this is likely to be postural hypotension rather than say, simple fainting or cardiac in origin. A typical history for someone with postural hypotension would be
- symptoms on, or soon after standing
- never occurs sitting or lying (except when being lying for some time or very severe when it may occur on sitting up or any postural change)
What happens when we stand up?
When we stand, our bodies should respond to keep our blood pressure the same. This requires three things
- normal plasma volume i.e. not dehydrated (younger people compensate well for this)
- intact baroreceptors and reflexes: these are pressure sensors around the body which detect changes in pressures and tell the blood vessels how to respond.
- venomotor tone: i.e. the ability of blood vessels to respond to changes in blood flow
Orthostatic Hypotension: Mechanisms, Causes, Management. Low & Tomalia. J Clin Neurol. 2015
When we stand, we need a higher pressure to overcome gravity and pump blood to the brain, which is now further from the floor. This drop in blood pressure should be recognised by the baroreceptors which then send signals to the heart to increase the heart rate and cardiac output (stronger beat) and to the arteries and veins to change their tone to increase blood pressure through constriction. This is done via the autonomic nervous system.
An important area of blood supply for this, is not actually the lower limbs, but the abdominal blood supply (splanchnic mesenteric), which holds a large blood supply and has many baroreceptors.
Causes
Acute
Can be ‘acute’ secondary to dehydration: decreased intake, diuresis, vomiting, bleeding.
Medications
Medications which alter or impair the normal physiological responses above can have the side effect of postural hypotension
- Heart rate control drugs such as beta blockers may impair heart rate response
- Blood pressure tablets may prevent blood vessel tone from responding normally in attempt to keep blood pressure down
- Diuretics like furosemide or spironolactone may over-dehydrate
Often concern about stopping antihypertensives and this should always take into account the cardiac and cerebrovascular risk of the individual alongside their prognosis. Two studies which support the safety of withdrawal and are:
Deprescribing antihypertensive treatment in nursing home patients and the effect on blood pressure. Gulla et. al, Journal of Geriatric Cardiology 2018
Lower blood pressure during antihypertensive treatment is associated with higher all-cause mortality and accelerated cognitive decline in the oldest-old. Data from the Leiden 85-plus Study. Streit et al. Age and Ageing 2018
Autonomic dysfunction
Conditions like diabetes and parkinsons disease can affect the autonomic nervous system directly, which then impairs normal responses to standing. As can recent surgery etc.
Drugs for parkinson’s disease may also exacerbate this further.
Some autoimmune conditions can cause autonomic dysfunction too (diabetes probably being the commonest.)
Measuring Postural Blood Pressure
RCP produced guidance with downloads for how to measure postural BP as part of inpatient falls quality improvement project.
- Ensure you are able to stand the person, get help beforehand if you think you might need it
- Ideally use a manual sphygmomanometer if possible
- Lie patient down for 5 minutes
- Measure blood pressure
- Stand them up and measure in the first minute
- Repeat at 3 minutes.
- If BP is still dropping, repeat and keep checking until it resolves.
- Repeat if symptoms change at any point.
Most likely to be low at 30 seconds.
Review of non-pharmacological interventions
Many hypothesis around. Essentially there are no real large studies that can guide, so while there may be ‘no evidence’ this doesn’t necessarily mean they won’t work for individuals so often worth trying a few out to see if they suit, – most pretty non-invasive.
Abdominal Binders
- ‘Corsets’ beneficial in about 50% usefulness comes down to practicalities.
- Compression stockings – full length, grade 2 and above. Logistically quite tricky to put on or to tolerate the high pressures exerted. Standard TEDS unhelpful as amount of blood in calves is relatively small.
Bolus of Water / Bed Elevation.
- Drinking water – conflicting evidence: Needs to be a fluid bolus, sufficient to change the osmolality of portal blood supply and induce an autonomic response in blood pressure. A 500ml (pint) of water within 5 minutes with benefit lasting around 90 minutes. Useful if predictable timing e.g. first thing in the morning.
- Tilting the head of the bed – theory is lower renal perfusion pressure leading to decreased diuresis and therefore fluid retention, to maintain a peripheral capillary pressure for when stand up. Another benefit is avoiding supine hypertension from lying flat in someone with impaired baroreceptor responsiveness. 10 degrees on the flat (by the height of a brick), 30 degrees in the day.
Caffeine / Countermanouvres
- Caffeine: no evidence
- Countermanouevres:
- Physical manoeuvres to increase blood return to heart by increasing peripheral resistance: standing on toes, pelvic and abdominal clenches
- Crossing legs and squeezing, squeezing buttocks / thighs / calves while they stand
- Standing up slowly
- 24 patients were observed standing slowly, at normal speed and quickly and showed significant reduction in blood pressure drops.
Standing Up Slowly Antagonises Initial Blood Pressure Decrease in Older Adults with Orthostatic Hypotension. de Bruïne Eline S. Gerontology 2017
Drugs – to discuss later
Education for self management / Exercise
- To understand that their blood pressure responses are not normal and they need to find ways to adapt their lives to live with it in the longer term.
- STOP what you’re doing: when you recognise symptoms coming on
- SIT down: allow blood pressure to recover
- DRINK some water: most modifiable factor in the immediate term
- THINK about triggers: recognise patterns to manage
- Exercise: a course of moderate exercise can improve orthostatic tolerance and symptoms. Also can help with practising standing slowly to avoid symptoms and getting up from floor.
Fluid & Salt
- Ensure measures taken to increase fluid intake as much as possible (hydration episode)
- Increased salt intake: theory is to help retain water and blood pressure, no evidence it works.
Pharmacological interventions: Drugs
Fludrocortisone
- aims to promote fluid retention to aid blood pressure
- recent NICE review of the literature showed only 2 studies eligible to be included, with a total of 19 people (6 diabetic men and 13 people with PD).
- i.e. Not enough evidence of benefit.
Midodrine
- peripheral arterial vasoconstrictor (i.e. need to use with caution in those with IHD or peripheral arterial disease)
- NICE evidence summary: now recommended for use where other measures have failed.
- Drop out of taking it was 28% within a year.
- Takes an hour to work, shouldn’t lie down within 6 hours
- Recommend trial 2 weeks and review
- Monitor BP
Comprehensive Geriatric Assessment: 695 Finnish people, aged ≥75 years, were randomised to annual CGA or to usual care, 96% resided in their own home. Over the following 3 years, compared to baseline there was a 7% reduction in the prevalence of OH in the CGA cohort compared to an increase of 8% in the standard care group
New Horizons in Orthostatic Hypotension, Frith & Parry, Age & Ageing 2017
Curriculum Mapping:
This episode covers the following areas (n.b not all areas are covered in detail in this single episode):
| Curriculum | Area |
| NHS Knowledge Skills Framework | Suitable to support staff at the following levels:
|
| Foundation curriculum | 10 Recognises, assesses and manages patients with long term conditions
12 Requests relevant investigations and acts upon results 13 Prescribes safety |
| Core Medical Training | The patient as central focus of care
Relationships with patients and communication within a consultation Blackout / collapse – detect orthostatic hypotension Unsteadiness / Balance disturbance Cardiology |
| GPVTS program | Section 2.03 The GP in the Wider Professional Environment
Section 3.05 – Managing older adults
|
| ANP (Draws from KSF) | Section 7.11 Syncope, pre Syncope, dizziness
7.20 Falls. Dizziness, syncope |
| Geriatric Medicine Higher Specialist Training | 28 Acute conditions (presyncope)
29 Chronic conditions (dizziness) 46 Falls and Syncope |
| PA Matrix of conditions | Cardiology – Hypotension – orthostatic/postural |






1 Response
[…] example of this (that we have discussed previously in episode 6.02) is someone experiencing postural hypotension due to antihypertensives. We might accept a […]