Episode 3.05 Mouth Care and Oral Health
Presented by:
Dr Iain Wilkinson (Consultant Geriatrician East Surrey Hospital)
Dr Jo Preston (Consultant Geriatrician St George’s Hospital)
Mili Doshi (Dentist, East Surrey Hospital)
Claire Watson (Nurse, BSUH)
Broadcast date: 11th April 2017
Click here for a downloadable PDF version of this infographic
CPD log
Click here to log your CPD online and receive a copy by email.
Episode 3.05 Mouth Care and Oral Health – Show Notes
Click here to download a PDF version of the show notes
Learning Outcomes
Knowledge:
- Understand links between oral health and general health
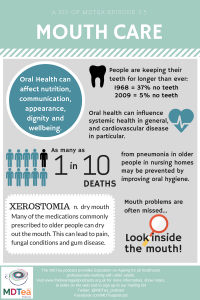
- Be aware of the importance of supportive mouth care and the impact on nutrition, communication, appearance, dignity and wellbeing
- Understand the importance carrying out regular mouth assessments
Skills:
- To be able to identify when patients have oral related problems that are impacting on their everyday life
- To be able to appropriately manage oral conditions
Attitudes:
- “Put the mouth back into the body”
- To prioritise oral health in both acute and community care
Key Points from Discussion
1. The population and our mouths
As we know we are an ageing population with increasing morbidities and increased care needs. Our mouths our also changing, and we are keeping our teeth for longer, sometimes called the ‘heavy metal generation’ with lots of dental work. Mouths with teeth needs meticulous care to maintain, and while this isn’t a problem if we live well, for those who do not it can become a problem. Many people as they get older for medical, physical or cognitive reasons will rely on another person to recognise they need help with mouth care and then provide the mouth care. There is little widespread training, and unfortunately mouth care is something across acute and community settings that is not prioritised and can lead to unnecessary pain and suffering.
1968 = 37% No teeth
2009 = 5% No teeth (likely to have reduced further)
Adult Dental Health Survey 2009
World Health Organisation. Oral Health.
Polypharmacy and many systemic diseases can be a cause of acute oral ulceration, candidal infection and xerostomia, which can be debilitating for patients (Dagli R. & Sharma A. 2014).
Dry mouth, or Xerostomia is very common and there are many potential causes:
- Systemic conditions such as Sjögrens and diabetes
- Medications
- There are over 400 medications that can cause dry mouth, including common medications such as NSAIDS, diuretics and antimuscarinics.
- Many drugs taken by the older population result in xerostomia, and this absence of saliva can cause a whole host of problems from pain to increase in fungal conditions and gum disease
- Sleeping with the mouth open
- Oxygen therapy
Consider pharmacy input in reviewing medications and recommendation of oral moisturising gels. Consider switching to humidified oxygen.
2. Barriers to oral care
- Nurses have very limited training and there is often no continuing CPD in mouth care. A survey at SaSh found less than 50% of nurses had had mouth care training.
- Nursing assistants often have no training and oral health was not included in the care certificate introduced in 2014.
- Junior doctors have very limited oral health training at both undergraduate and postgraduate level (McCanna et al., 2005)
There is a wealth of research that investigates the reasons why oral care is not provided for hospitalised patients. Barriers that have been reported by nurses include a lack of knowledge (Preston et al., 2016), a lack of training and time constraints (Adams, 1996) as well as a lack of equipment (Stout et al., 2009). Other studies have reported that some nurses have a “disagreeable” attitude towards oral care procedures (Wardh, et al., 1997) and that the nurse’s attitude towards their own orodental care may influence the oral care advice that they give to patients (Preston et al., 2000)
3. Oral health and general health
There are more bacteria in your mouth than people in the world! Plaque must be mechanically removed with a toothbrush daily. (Avoid rinsing for 30mins after brushing)
There are links between poor oral health and many systemic conditions including CVD and diabetes. There is increasing evidence of link between oral flora and aspiration pneumonia.
Evidence summary: the relationship between oral health and pulmonary disease
Manger et al., 2017
Cardiovascular disease
Oral health has an influence on systemic health in general and on cardiovascular disease in particular. Therefore, we should promote oral health in general and periodontal health in particular as part of a healthy life style and hence as an important component of CVD”
European Society of Cardiology 2010
(See also Tonetti et al., 2013)
Diabetes
- In a 5 year prospective study of 2,974 non-diabetic individuals, people with periodontitis had 5-fold greater ∆HbA1c (0.11%) over 5 years compared to those with no periodontitis (0.02%)
Aspiration pneumonia
- Oral health is associated with aspiration pneumonia in older adults in both acute and care settings (Sarin et al., 2008)
- A systematic review found the removal of dental plaque reduces the incidence and mortality of pneumonia (Scannapieco et al., 2003)
- Approximately one in 10 cases of death from pneumonia in elderly nursing homes may be prevented by improving oral hygiene (Sjögren et al., 2008)
- Oral hygiene including chlorhexidine mouth rinse/gel reduced ventilator-associated pneumonia by about 40% (Shi et al., 2013)
A chance to identify head and neck cancer
- Head and neck cancer is the fourth most common cancer in the UK for men and the 12th most common for females (2014)
- Since the late 1970s oral cancer incidence rates have increased by 92% in the UK and numbers are expected to rise by a further 33% between 2015 – 2035. 1 in 75 men and 1 in 150 women can expect to be diagnosed with oral cancer during their lifetime. (Cancer Research UK)
- The most common intraoral site for head and neck cancer is the tongue, with squamous cell carcinoma of the tongue being the predominant malignancy (Loganathan et al., 2016)
- When tongue cancer is diagnosed early, 5 year survival outcomes range between 75-89% (Ganly et al., 2011 )
- Late diagnosis of oral cancer can significantly decrease 5-year survival rates (NIDCR)
4. Dignity
Losing dentures is an underreported problem and it can be very difficult to get new dentures for hospital inpatients. Many hospitals do not have an in-house service, and even when there is, it takes 6 weeks to make a new denture.
Losing dentures can be very distressing for patients, and has an impact on both nutrition and dignity. Removal of dentures can change the look of someone’s whole face, and they may feel embarrassed to have visitors, or struggle to engage with rehab.
5. MDT roles in oral care
Every member of the MDT is involved in some way in oral care.
Pharmacy
- Rationalising medications that can contribute to dry mouth
- Dry mouth moisturising gels for dry mouth
- Alcohol free mouth washes
- Alternative medicines that need less saliva – consider liquid or dispersible forms (eg calcium tablets often get stuck in mouth, patient cannot swallow)
SALT
- Recognize common oral problems during assessment- work with nursing staff to optimise mouth care
Nurses and nursing assistants
- Provide mouth care
- Day to day review and assessment, refer if necessary
Physiotherapists
- May be the person that identifies issues in the mouth when carrying out a chest assessment
Dietitians
- May come across patient who are not eating due to oral problems
Occupational therapists
- Can help with aids so that people can hold a toothbrush.
Doctors
- Look in the mouth!
- Learn to identify common oral conditions and treat them
Resources
- Mouth care assessment guide
- How to do an oral assessment
- more resources here
NICE guidance July 2016- oral health in care homes
Other resources mentioned in this episode:
If you have some links or resources you’d like to share, get in touch and we’ll add them here. Twitter @MDTea_podcast Facebook www.facebook.com/MDTea or email thehearingaidpodcasts@gmail.com
Curriculum Mapping: This episode covers the following areas (n.b not all areas are covered in detail in this single episode):
| Curriculum | Area |
| NHS Knowledge Skills Framework | Suitable to support staff at the following levels:
Personal and people development level 1-3 Service improvement level 1 |
| Foundation Curriculum 2012 | 2.1 Treats patient as centre of care
6.1 Lifelong learning 6.2 Evidence and guidelines 7.3 Diagnosis and clinical decision making 7.9 Interface with different specialties and with other health professionals 10.5 Health promotion, patient education and public health |
| Foundation Curriculum 2016 | 2. Patient centred care
4. Self-directed learning 6. Interface with other healthcare professionals 11. Diagnosis, Clinical management 13. Review of prescriptions |
| Core Medical Training | Common competences:
Symptom based competences: Abdominal swelling and constipation System specific competences:
|
| GPVTS program | Section 3.01 Healthy People: promoting health and preventing disease
Section 3.05 – Care of older adults
|
| ANP (Draws from KSF) | Section 5. KSF HSB2 Level 4
Section 7.30 Problems with mouth Section 13. Safe prescribing Section 20. The patient as central focus of care |
| PA Matrix of conditions | Conditions in Category 1A:
7.3 Mouth/Throat Disorders |
Feedback We will add feedback to this as we receive it! The website will have the most up to date version always available: www.thehearingaidpodcasts.org.uk/mdtea Find Us! To listen to this episode head to our website, itunes or stitcher. Give us feedback by emailing us, via twitter or facebook. Check out our cool infographic A sip of… summarising 5 key points on topic. It’s made for sharing!






