Episode 3.03 Preventing Pressure Ulcers
Presented by:
Dr Iain Wilkinson (Consultant Geriatrician East Surrey Hospital)
Dr Jo Preston (Consultant Geriatrician St George’s Hospital)
Faculty:
Clare Watson (Nurse, Brighton and Sussex University Hospitals)
Wendy Grosvenor (Dementia Nurse Specialist and Lecturer at University of Surrey)
Broadcast date: 14th March 2017
Click here for a PDF version of the infographic
CPD log
Click here to log your CPD online and receive a copy by email.
Episode 3.3 Preventing Pressure Ulcers – Show Notes
Click here for a PDF version of the show notes.
Learning Outcomes
Knowledge:
- To recall the underlying proposed pathophysiology of pressure sore development
- To understand why certain body areas are higher risk for the development of pressure injuries
- Develop understanding of the requirements to reposition and positions
- To have a better understanding of the influences of the ageing process on pressure sore risk
Skills:
- To be able to recognise when a person is at risk of pressure damage to their skin
Attitudes:
- Recognise the influence of personal choice / capacity in terms of pressure sore risk – e.g fabulous shoes!
Definitions:
You will hear the following terms used for describing pressure injuries including pressure ulcers, pressure sores, decubitus ulcers and bedsores (Beldon, 2006).
“A pressure injury to the skin and/or underlying tissue, usually over a bony prominence, as a result of pressure, or pressure in combination with shear”. (EPUAP, 2009).
In the UK all pressure ulcers should be documented and graded using the international recognised grading system EUPAP (NICE) as standard.
There is confusion between moisture lesions and pressure injuries: see the table below for clarification.
| Pressure injury | Moisture lesion | |
| Causes | Evidence/history of pressure, shear or friction | Skin obviously moist, history or incontinence |
| Position | Usually over a bony prominence unless compressed with equipment such as catheter or oxygen mask | Not over a bone, frequently in the natal cleft and/or over buttocks. May present as ‘kissing’ or copy lesion with the shape /pattern on both buttocks |
| Shape | Usually distinct shape with obvious edges, 1 or 2 wounds | Frequently multiple wounds with diffuse edges |
| Depth | From superficial to deep, may be down to bone | Usually superficial – unless it becomes infected |
| Necrosis | Frequently necrotic tissue present as hypoxia causes necrosis | No necrosis |
| Edges | Distinct edges, may be rolled or raised in chronic stages | Edges may be difficult to determine, jagged edges are seen in moisture lesions that have been subjected to friction |
EPUAP/NPUAP (2009) Prevention and treatment of pressure ulcers: quick reference guide (no longer available)
For 2014 guide click here
Key Points from Discussion
How does pressure injury occur?
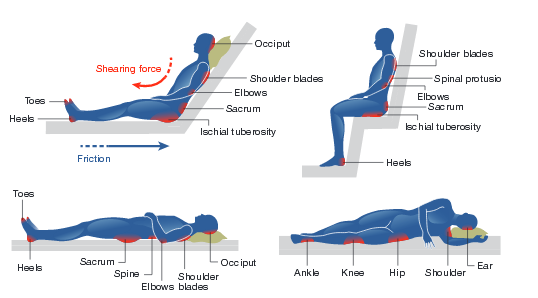
- Pressure ulcers usually occur over a bony prominence, such as the sacrum, ischial tuberosity and heels. However, they can appear anywhere that tissue becomes compressed, such as under a plaster cast, splint, arm sling, crutches – or under glasses / nasal cannulae.
- This occurs when the soft tissue of the body is compressed between a bony prominence and a hard surface. This occludes the blood supply, leading to ischaemia and tissue death.
- The forces of pressure are further exacerbated by moisture, and factors relating to the individual’s physical condition, such as altered mobility, poor nutritional status, medication, and underlying medical conditions.
Patients should be encouraged to move themselves, where possible, but others may require assistance.
- Repositioning should be considered for all those deemed to be at risk of pressure ulceration and patients should be offered an appropriate support surface to help prevent pressure damage.
- If the pressure is unrelieved for a long period of time, the damage will extend to the bone (top to bottom model for pressure sore development)
- The bottom-to-top model suggests that damage begins at the bone and works up through the muscle toward the skin, with visual assessment of the skin giving no indication of the extent of underlying tissue damage. Neither really talks about the role of re-perfusion injury to the skin
Either way…
-
- A cone-shaped ulcer is created, with the widest part of the cone close to the bone, and the narrowest on the body surface.
- This may be seen as a non-blanching erythema, or an area of superficial skin loss on examination suggesting minimal involvement at the surface, but providing no indication of how extensive the tissue damage may be (Nixon et al, 2007).
The prevalence of pressure ulcers is 1 of the 4 common harms recorded in the NHS Safety Thermometer, a local improvement tool for measuring, monitoring and analysing patient harms across a range of settings, including care homes, community nursing and hospitals on a monthly basis (NICE).
Who is at risk of developing a pressure ulcer?
NICE list the following as factors that should be considered;
- General health
- Age
- Reduced mobility
- Nutritional status
- Incontinence
But recommend using the Waterlow scoring system to assess risk for pressure damage.
| Extrinsic factors | Pressure
Shear (when skin is being pulled in 2 different directions – i.e skin ‘stuck’ to sheet and gravity pulling body down) Friction (the rubbing together of two surfaces) Moisture |
| Intrinsic factors | Reduced mobility
Impaired sensation Acute/Chronic/Palliative illness Pyrexia Medication –Steroids Age Level of consciousness and cognitive state Dehydration Incontinence History of pressure ulcers Pain – preventing repositioning Vascular disease Malnutrition |
As skin ages:
- The integrity alters as the epidermis gradually becomes thinner (Baranoski and Ayello, 2004; Voegeli 2007), making the skin more susceptible to damage from the mild mechanical injury forces such as moisture, friction and trauma (International Review, 2010).
- Flattening out of the dermo-epidermal junction, which makes it more fragile and more susceptible to shearing forces. This can cause stretching of the skin and damage to blood vessels (Voegeli, 2007).
- There is an estimated 20% reduction in the thickness of the dermis, which results in the paper-thin appearance, commonly associated with the elderly (Haroun, 2003).
- Thinning of the dermis sees a reduction in the blood vessels, nerve endings and collagen with the inability to protect the body (Baranoski and Ayello, 2004). In addition, older adults may not be able to detect temperature changes readily, making them more susceptible to the cold and hypothermia.
Limited research really into the actual molecular mechanisms of pressure ulcer development. One study looked at a model using aged and young skin and concluded… “that aging contributes to rapid morphological changes and decrease in inflammasome proteins in response to tissue damage, suggesting that a decline in the innate inflammatory response in elderly skin could contribute to pressure ulcer pathogenesis.”
High risk areas
High risk areas are anywhere that comes into contact with pressure, however this is typically over bony prominences (see below)
Wounds UK, Care of the older person’s skin: Best practice statement (Second edition)
Grading pressure injury
There are a number of grading systems to use – the key point is to use whatever you hospital / trust / practice uses and be familiar with the system.
They all tend to start with non-blanching erythema and then progress to deep tissue loss (down to bone).
There is a good example here.
Preventing pressure injuries
The only way to prevent pressure damage is to take away the pressure by repositioning.
Frequency
The NICE guidelines recommend that patients who are assessed as being at risk should reposition frequently but at least every 4 hours. For those who are not at risk every 6 hours. Although other documents recommend more frequent changes, every 2 hours including wound UK (2012)
Looking at the evidence the NICE guidelines regarding positioning come from 6 low quality studies and their methods were not comparable. One study, which was carried out 27 years ago, used, rolled up towels as adjuncts which we know, from clinical practice, does not reduce pressure injuries as the towel is still applying pressure. Another study, published 12 years old, used sheepskin blankets and water mattresses.
Anyway, having looked at all 6 studies the findings are not very precise with regards to frequency of positioning.
From experience, 2 hours seems more acceptable for those with an increased risk of pressure injury or who already have a pressure injury.
Position
NICE guidelines don’t recommend specific positions.
In a small Swedish study carried out in the hospital setting. The researchers used instruments to measure blood flow and rather interestingly what they found was the 30’ lateral tilt decreased blood flow over trochanter, especially to the superficial skin.
These findings do contradict other studies but the participants where older adults who were inpatients in hospital, suggesting they would have had other risk factors that we associate with the older adult demographic and would have been clinically unwell.
Devices
There are lots of mattresses on the market. Consider upgrading and downgrading dependent upon patient’s clinical needs. Mattresses don’t take the pressure away- they just provide a bit more time before repositioning is required, about 7-15 minutes.
Resources
If you have some links or resources you’d like to share, get in touch and we’ll add them here. Twitter @MDTea_podcast Facebook www.facebook.com/MDTea or email thehearingaidpodcasts@gmail.com
SSKIN Bundle in pressure prevention
The SSKIN bundle concept was an American healthcare initiative; in America all pressure injuries are listed as ‘never events’. Representatives from the Institute for Healthcare Improvement and Ascension Health developed a blueprint for change in PU prevention.
- Skin
- Surface
- Keep moving
- Incontinence
- Nutrition
Curriculum Mapping: This episode covers the following areas (n.b not all areas are covered in detail in this single episode):
| Curriculum | Area |
| NHS Knowledge Skills Framework | Suitable to support staff at the following levels:
Personal and people development level 1-3 Service improvement level 1 |
| Foundation Curriculum 2012 | 2.1 Treats patient as centre of care
6.1 Lifelong learning 6.2 Evidence and guidelines 7.1 Makes patient safety a priority in good clinical practice 7.3 Diagnosis and clinical decision making 7.9 Interface with different specialties and with other health professionals |
| Foundation Curriculum 2016 | 2. Patient centred care
4. Self-directed learning 6. Interface with other healthcare professionals 11. Clinical management 19. Patient safety |
| Core Medical Training | Common competences:
Symptom based competences: Abdominal swelling and constipation System specific competences:
|
| GPVTS program | Section 3.05 – Care of older adults
|
| ANP (Draws from KSF) | Section 7.4 Common types of leg and pressure ulceration, acute ischaemic limb, surgical and other wounds in older patients.
Section 7.13 Iatrogenic problems including consequence of hospitalisation and bed rest Section 20. The patient as central focus of care |
| PA Matrix of conditions | Conditions in Category 1A:
12 12 6 Decubitus ulcers/leg ulcers |
Feedback We will add feedback to this as we receive it! The website will have the most up to date version always available: www.thehearingaidpodcasts.org.uk/mdtea Find Us! To listen to this episode head to our website, itunes or stitcher. Give us feedback by emailing us, via twitter or facebook. Check out our cool infographic A sip of… summarising 5 key points on topic. It’s made for sharing!






2 Responses
Very impressive blog.
Interesting article right on the subject.
[…] S3E3 – Pressure Ulcer Prevention […]