Episode 2.5 – UTIs
MDTea Episode 2.5 – Urinary Tract Infections (UTIs)
Presented by: Jo Preston (Consultant Geriatrician at St George’s Hospital) and Iain Wilkinson (Consultant Geriatrician at East Surrey Hospital).
Core Faculty: Claire Watson (Practice Development Nurse at Royal Sussex County Hospital), Adam Buckler (Pharmacist at East Surrey Hospital) and Gabor Szekely (GP in Brighton).
Guest Faculty: Amy Heskett (Community Geriatrician in Kent).
In this episode we talk about UTIs, how to diagnose them accurately and avoid over diagnosis. We also explore how to prevent and manage UTIs, including investigations (beyond the dreaded dip!)
Broadcast date: 18th October 2016
Here is a sip of this week’s MDtea
CPD log
Click here to log your CPD online and receive a copy by email.
Show Notes – Episode 2.5 – Urinary Tract Infections
(click above to download)
Learning Outcomes
Knowledge
- To know how the symptoms of a UTI may differ in older adults
- To recall some complications of UTIs in older adults
- To understand the contributing factors that make older adults susceptible to UTI
Skills
- To be able to interpret the common investigations in the diagnosis and management of UTIs
- To know how to perform a bladder scan looking for retention of urine following micturition.
Attitudes
- To not assume all lower urinary tract symptoms are due to UTIs
- To question a diagnosis of UTI when it has been made without full facts
So what is a UTI?
- An infection of urinary tract (anywhere from the kidneys down to urethra via the bladder)
- Recurrent urinary tract infection is defined as three episodes of urinary tract infection (UTI) in the previous 12 months or two episodes in the last six months.
- It is not!
- Acute trimethoprim deficiency! @sean9n
- The root source of all ‘confusion query cause’ [ep 2 on delirium]
- Proven or diagnosed by a ‘positive’ dipstick alone
Symptoms:
- The common (specific) symptoms are: Dysuria (pain on urination), urinary frequency (‘cystitis’), blood or pus in urine, feeling of incomplete emptying and or lower abdominal pain
- A UTI can be a cause of new urinary incontinence – and should be excluded when treating UI – particularly OAB symptoms (infection irritates lining of bladder) [ep3 on continence]
- There may be a number of non-specific symptoms which could be common to any infection: delirium, reduced appetite, newly reduced mobility leading to falls, nausea.
Making the diagnosis:
- A criteria for diagnosing UTIs in Nursing Home residents (without catheters) has been developed by Infectious Disease Consensus Groups:
- Bacteriuria plus pyuria (i.e. >10 WBC/ml)
- AND 2/3 of:
- Dysuria
- Change in mental state
- Change in character of urine
A nice review of this is here on a BMJ podcast.
Complicated UTI:
Essentially when there is something else going on – Important in terms of thinking about the cause but also knowing this may affect your choice of treatment.
- Structural abnormality e.g. cystocele / fistula (Men who have symptoms of an upper urinary tract infection should be referred for urological investigation – as per NICE QS 90)
- Iatrogenic: catheter
- Voiding dysfunction e.g. high post void residual (talk through how to do), reflux into ureters
- Obstruction e.g. stone or bladder outflow obstruction, constipation
- Diabetes / immunosuppression*
To dip or not to dip?
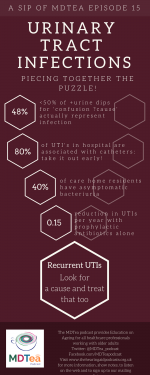
- In conjunction with symptoms, dipsticks can have a sensitivity around 77% – so not too bad!…however – as a ‘screening test’ in absence of actual urinary symptoms, and just in someone presenting with confusion it is 44% – worse than flipping a coin!
- The frequency of positive urine dips in institutional care is very high – this is due to the fact that upto 50% of females in nursing homes, have asymptomatic bacturia – in non-care home residents this is a little less – ranging from 6 to 16% in females aged 65-90.
- One study found that the negative predictive value of a urine dipstick was 100% for Nursing Home residents (i.e. this means that you can have a very high confidence that a negative result is true (i.e there is no infection)).
- When a person has a urinary catheter in situ – the changes of this being colonised with bacteria is around 100%! – and so urine dipsticks are useless if someone has a urinary catheter – so don’t send one and certainly don’t treat an asymptomatic patient on the basis of a dipstick!
Here is some good and easy to follow guidance from the British Geriatrics Society – However sepsis trumps all and if your patient is septic – start the most appropriate antibiotic rapidly and follow the sepsis guidance (being very frail puts you into a higher risk group). (NICE Sepsis guidance NG 51)
| Patient history | Symptoms | Signs | Urine dip |
| Clear and unambiguous | New onset of frequency, dysuria; | Abdominal pain Haematuria
Offensive smelling urine Fever |
Negative – seek other cause. Do not send MSU |
| Positive for leucocytes and nitrites – likely UTI, send MSU and treat | |||
| No urinary symptoms | Do not dip urine, do not send MSU | ||
| Lacking because of communication barriers | Increased confusion, apathy, irritability (delirium), reduced mobility, off food | Abdominal pain Haematuria
Offensive smelling urine Fever |
Negative – seek other cause. Do not send MSU |
| Positive for leucocytes and nitrites – likely UTI, send MSU and treat | |||
| Leucocyte positive only – seek alternative diagnosis
Nitrite positive only – send MSU and start treatment |
When starting treatment always think about the need for an MSU – which should ideally be a sample of urine taken from the middle of the urinary stream (so a clean catch – not something taken from a pad etc. if at all possible!).
Treatment
Follow your local guidelines for antibiotic choice – Treatment is generally 3 days for women and 7 days for men.
Other things to think about:
- Cranberry juice: inconclusive evidence for both juice and supplements (Cochrane review here)
- Lemon barley (can help with pain of cystitis but does not remove infection!)
- Prophylactic antibiotics: usually not favoured…. Can reduce infections by 0.15 events per year but lots of side effects found in study.
See also NICE quality standard 90.
- Topical vaginal oestrogens (useful when there is vaginal atrophy and recurrent UTIs): Available as cream or ring pessaries (latter changed every 12 weeks), former needs manual dexterity and capacity to consent to potentially invasive treatments. Can cause local irritation in up to 20%. Sometimes dysuria is related to this rather than a UTI anyway.
Cochrane review oestrogen treatment and UTI
Considerations for community treatment vs hospital admission:
- Able to be treated with oral antibiotics + able to be compliant with taking these?
- Able to maintain adequate hydration (remember to drink plus access to drinks)
- Access to bathroom (frequency and potential decrease in mobility): or commode?
- Decompensation of other conditions may occur: can these be managed at home too?
Curriculum Mapping:
This episode covers the following areas (n.b not all areas are covered in detail in this single episode):
| Curriculum | Area |
| NHS Knowledge Skills Framework | Suitable to support staff at the following levels:
|
| Foundation Curriculum 2012 | 7.2 History and examination
7.3 Diagnosis and clinical decision-making 11. Investigations |
| Foundation Curriculum 2016 | 11. History
11. Physical examination 11. Diagnosis 12. Interpretation of investigations |
| Core Medical Training | Common competences:
Symptom based competences:
System specific competences:
Investigation competences:
|
| GPVTS program | Section 3.05 – Managing older adults
|
| ANP (Draws from KSF) | Section 4 – History taking skills
Section 6 – Clinical Examination Section 7.8 – Urine retention, incontinence and infection Section 8 – Atypical presentations |
| Physician Associate Matrix of conditions | 1A conditions: 11. Cystitis |
| College of Paramedics Curriculum Guidance | C2.6.8 Formulate a diagnosis from the analysis of clinical examination, history and vital signs assessment findings.
C 2.6.9 Identify the need for further assessment, intervention or referral to specialist or advanced paramedics, or other services, care pathways or agencies. |