Episode 1.10 Rehabilitation Potential
MDTea Episode 10: Rehabilitation Potential
Presented by: Jo Preston (Consultant Geriatrician at St George’s Hospital) and Iain Wilkinson (Consultant Geriatrician at East Surrey Hospital).
Core Faculty: Sarah Jane Ryan – Physiotherapist, Tracy Szekely – Occupational Therapist and Pam Trangmar – Physician Associate.
This episode explores the evidence base for rehabilitation in older adults, in particular those with cognitive impairment. We also look at the question of what we mean by rehabilitation potential.
Click here for the show notes for this episode.
Here is a Sip of MDTea for this episode.
CPD log
Click here to log your CPD online and receive a copy by email.
Episode 10 Show Notes
Rehabilitation Potential
___
Presented by: Dr Jo Preston & Dr Iain Wilkinson
Faculty:
Sarah- Jane Ryan – Physiotherapist, Tracey Szekely – Occupational therapist, Pamela Trangmar – Physician Associate
Broadcast Date: 24th May 2016
Learning Outcomes
Knowledge:
To understand the concept of rehabilitation potential and how multiple members of the MDT have an impact on this.
Skills:
To use the concept of rehabilitation potential with your patients and MDT.
Attitudes:
- To understand person centered care and how this may impact upon rehabilitation potential
Definitions:
Formal / Scientific Definition:
Geriatric rehabilitation is a multidisciplinary set of evaluative, diagnostic, and therapeutic interventions whose purpose is to restore functional ability or enhance residual functional capability in elderly people with disabling impairments.
Boston Working Group on Improving Health Care Outcomes Through Geriatric Rehabilitation
Practical Definition:
Restoration of the individual to his or her fullest physical, mental and social capability
Rehabilitation of older people. Young et. al BMJ, 1998
Really started by Marjory Warren – who pioneered the idea of rehabilitation in older patients.
Marjorie Warren the mother of geriatric medicine
Not everyone will be suitable for rehabilitation, for example in the very end stages of a disease process, but we feel rehabilitation should be offered to all who may benefit.
- Assuming that most people have rehabilitation potential is a good place to start but may be unrealistic for some patients.
- Conversely, some people may appear to have little to gain from pure functional perspective but may be difference between some independence (can be physically or psychologically) or not – for example a patient following a stroke who is making little overall progress but being able to transfer would greatly improve their quality of life.
Important to first know that older adults do have things to gain from rehab.
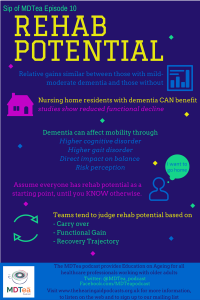
Rehabilitation in patients with dementia
There is often a debate though about patients who have dementia – the evidence though is lacking at the moment but slowly increasing.
Cochrane Review of Exercise Programs for People with Dementia. Forbes et. al 2015
The study below showed that a 12 week program of twice weekly small group exercise led to improvement in Berg Balance scale in nursing home residents all of whom had dementia, compared with those who did not participate..
Specifically looking at hospitalised patients:
Following a hip fracture – patients with mild to moderate dementia showed similar gains to other patients.
Rehabilitation specifically designed for geriatric inpatients has the potential to improve outcomes related to
- Function
- admission to nursing homes
- Mortality.
Rehabilitation Potential
Concept of rehabilitation potential is important but there is not a very good shared understanding of what rehab potential means between MDT members.
A thematic analysis suggests judgement of rehab potential was based on three areas.
- Carry over
- Functional gain
- Recovery trajectory
Judgement on these three factors in this article seemed then to affect the interactions between MDT members and patients e.g. Balancing optimism and realism
A literature review looking at the assessment and selection of patients in acute hospitals for their need for inpatient rehabilitation before discharge concludes that the assessment of patients in acute hospital for rehabilitation is an important skill and it has the potential to improve patient outcomes. There is however a need for further research in this area.
Rehabilitation differs from the purely medical model in 2 ways:
- Liaison between teams (the MDT) is absolutely imperative
- Learning is taking place by the patient and relatives and this is the key process that is taking place.
Both of these have a focus on communication and our take home message is that communication is the key skill in rehabilitation and talking to the patient, being honest with them about their progress and wishes for the future and communication with the rest of the team is so so key. Just because the patient may not be making progress in your area does not mean that they are not making important progress with another member of the team (e.g they may not be making progress in terms of mobility following their stroke but might be making really important functional gains in terms of personal care which will affect not only their quality of life and ongoing care needs).
Curriculum Mapping:
This episode covers the following areas (n.b not all areas are covered in detail in this single episode):
| Curriculum | Area |
| NHS Knowledge Skills Framework | Suitable to support staff at the following levels:
|
| Foundation Curriculum 2012 | 1.3 Continuity of care
1.4 Team working 2.1 Patient as centre of care 7.9 Interactions with different specialities and other professions 10.1 Manages patients with long-term conditions 10.4 Discharge planning |
| Foundation Curriculum 2016 | 2. Patient centred care
4. Self-directed learning 6. Interface with other healthcare professionals 10. The frail patient 10. Support for patients with long term conditions 11. Discharge planning |
| Core Medical Training | Core competences:
Symptom based competences:
System specific competences:
|
| GPVTS program | Section 2.03 The GP in the Wider Professional Environment
Section 3.05 – Managing older adults
|
| ANP (Draws from KSF) | Section 6. Clinical examination
Section 7.13 Iatrogenic problems including consequence of hospitalisation and bed rest. Section 7.21 Dementia Section 17. Rehabilitation Section 18. Discharge |