9.04 Parkinson’s: Non-motor symptoms
Presented by: Iain Wilkinson, Jo Preston, Alice O’Connor
Broadcast Date: 17th March 2020
Social Media
Iain: BGS healthier for longer report…
www.bgs.org.uk/healthierforlonger
Learning Outcomes
Knowledge
- To understand the pathogenesis of Parkinson’s disease and the presence of both motor and non-motor symptoms
- To be able to identify troublesome non-motor symptoms and suggest options for management
Skills
- To be able to administer the non-motor symptoms questionnaire
Attitudes
- To understand the impact of non-motor symptoms of the quality of life of someone with PD
CPD Log
Show Notes
Definition
What are non-motor symptoms?
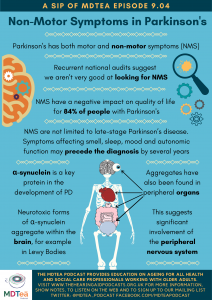
In PD there is a diverse range of symptoms which reflect the widespread neurochemical and neuroanatomical changes that occur throughout the course of Parkinson’s disease.
There is involvement of not only the dopaminergic nigrostriatal system, but also serotonergic and noradrenergic brainstem areas, cholinergic frontal and brainstem regions. These all lead to slightly different symptoms which can broadly be divided into those relating to movement (so called Motor) and those related not to movement (the non-motor).
Main Discussion
Pre-diagnostic phase
From observational and longitudinal studies, several non-motor features affecting smell, mood, sleep, and autonomic function have now been linked to the risk of the development of Parkinson’s disease and neurodegenerative diseases.
Other non-motor symptoms such as cognitive impairment, autonomic dysfunction, and sleepiness have been identified early in de novo, untreated Parkinson’s disease patients.
These are therefore important symptoms and PD can be thought of as a neuropsychiatric condition with motor symptoms (rather than the other way around, which was the common situation before).
Interestingly, Friedrich Lewy (1913) first described Lewy bodies in the dorsal motor nucleus of the vagus- and not the brain (would be Braak stage 2)
Todorova A, et al. Pract Neurol 2014;14:310–322
(NERD ALERT)
Key protein in PD is α-synuclein
- In PD, α-synuclein adopts a β-sheet-rich amyloid-like structure that is prone to aggregate. Indeed, misfolded α-synuclein is found within Lewy Bodies.
- different forms of α-synuclein are found in the PD brain – including unfolded monomers, soluble oligomers, protofibrils, and high molecular weight insoluble fibrils.
- Recent studies in rodents indicated that the most neurotoxic α-synuclein species is the early oligomeric form, rather than the mature insoluble fibrils.
- The oligomeric species of α-synuclein are capable of “seeding” and accelerating abnormal protein aggregation and it is proposed that this might be the mechanism underlying the spread of α-synuclein pathology in the brain
- However it’s not just the brain…
- α-synuclein deposition is observed in several peripheral organs, including the retina, the uterus, the bladder, the skin, parts of the cardiovascular system (predominantly in the aorta and heart ventricles), and the gastrointestinal system, particularly in the submandibular gland, stomach, and the bowels..
- This points to a significant involvement of the peripheral nervous system in PD and raises the question of whether α-synuclein pathology originates in the brain or in the periphery.
- α-synuclein deposition is observed in several peripheral organs, including the retina, the uterus, the bladder, the skin, parts of the cardiovascular system (predominantly in the aorta and heart ventricles), and the gastrointestinal system, particularly in the submandibular gland, stomach, and the bowels..
This book chapter explores the pathogenesis of PD very well – needless to say it’s quite complex and not a simple story!
Non Motor Symptoms are common:
In advanced PD, NMS are an important determinant of loss of independence and residential placement of people with PD (PwP).
NMS contribute substantially to the burden of PwP and their care partners – but the PD UK national audits show we don’t ask about them enough.
https://www.parkinsons.org.uk/professionals/uk-parkinsons-audit-transforming-care
There are a number of self completion questionnaires for NMS – personally I (Iain) like the Non-Motor symptoms questionnaire.
(MDT developed questions which were then trialled on patients with and without PD).
Kings-ISCIII grading by NMSQuest (can be performed by healthcare professional and based on patient responses using NMSQ)
Stage 0 (NMSQ: 0) – no non-motor symptoms
Stage 1 (NMSQ: 1–5) – mild NMS
Stage 2 (NMSQ: 6–12) – moderate
Stage 3 (NMSQ: 13–20) – severe
Stage 4 (NMSQ: 21–30) – very severe
In an online survey of patients and carers:
- More than half of respondents (PwP themselves or their care partners) reported:
- sleep problems or excessive tiredness (84%),
- cognitive challenges (76%),
- anxiety (65%),
- or depression (56%)
- Respondents also reported a high prevalence of hallucinations (40%) and delusions (23%)
- NMS had some, quite a bit, or very much of a negative impact on quality of life for PwP according to 84% of the respondents
- Overall nearly half of respondents (48%) indicated that NMS represent a greater challenge than motor symptoms.
- However, a greater percentage of care partners (354 respondents) reported that NMS were more or much more challenging than motor symptoms compared with responses from PwP 58% vs 32%.
- Despite the perceived impact of NMS, 50% of the respondents indicated that their friends and family had very little or no understanding of the impact of PD on daily living.
Perhaps also the cumulative effect is more important than the severity of one single item.
Key Messages: NMS are generally prevalent and highly burdensome within selected Asian PD populations living in countries. It is suggested that NMS-driven phenotypic heterogeneity is present in Asian patients, and compared to Western PD populations there might be variations in assessed NMS.
Symptoms are not easy to lump together but one article suggests the following classification which we think is helpful:
- Related to the disease process or pathophysiology
- Dopaminergic origin
- Non-dopaminergic origin
- Related to a partial non-motor origin (usually brainstem autonomic impairment with motor end result, such as constipation or diplopia)
- Related to non-motor fluctuations (cognitive, autonomic and sensory subtypes)
- Fluctuating
- Constant
- Related to PD drug therapy
- Specific symptoms (eg, hallucinations, delirium)
- Syndromes—impulse control disorders, dopamine agonist withdrawal syndrome, Parkinson’s hyperpyrexia syndrome (thermoregulatory failure, delirium)
- Possibly genetically determined
- Dementia in cases with glucocerebrosidase mutation
- Depression and sleep disorders in cases with leucine-rich repeat kinase-2 mutation
Todorova A, et al. Pract Neurol 2014;14:310–322
As PD progresses, it is common knowledge that a problem can occur known as the “on-off” phenomenon. The same can happen with NMS and can be equally disabling. Symptoms can be a worsening of something that is there already – or a new symptom that only comes during the off period.
NON-MOTOR SYMPTOMS THAT WORSEN DURING ‘OFF’ PERIODS
▸ fatigue
▸ depression
▸ anxiety
▸ inner restlessness
▸ impaired concentration/attention.
Todorova A, et al. Pract Neurol 2014;14:310–322
Some specific NMS
We will focus on a few NMS and look at the management plans.
The MDT has a significant role to play: SaLT, PD nurses, bladder and bowel services, PT, OT, medics and support groups.
Physical activity may be a suitable non-pharmacological therapy in PD. Global and specific NMS involving depression, apathy, fatigue, cognition, and sleep were significantly improved by some form of physical activity.
Sleep
- Excessive daytime sleepiness
- Common strategy:
- Sleep hygiene (regular daytime exercise, avoiding stimulants at bedtime, regular hours of sleep at night)
- Modafinil (subjective improvement)
- Might help / investigational
- Caffeine intake (contradictory data and tablets may be used)
- Sodium oxybate—taken at night, only under specialist supervision (potential for abuse)
- Selective histamine H3 receptor inverse agonist
- Pitolisant (in trial)
- Adenosine receptor antagonists—Istradefylline, Tozadenant
- Common strategy:
- Insomnia Sleep hygiene
- Common strategy
- Short-acting benzodiazepines
- Non-benzodiazepine hypnotics
- Zopiclone
- Tricyclic antidepressants
- Amitriptyline
- Might help / investigational
- Night-time apomorphine infusion or Rotigotine patch (may help in cases of insomnia due to severe nighttime rigidity, restless legs syndrome and ‘off’ periods)
- Common strategy
- REM sleep behaviour disorder
- Sleep in a safe environment while in bed, (remove all sharp and breakable objects)
- Clonazepam (usually used first line)
- Melatonin
- Pramipexole in combination with Clonazepam (one successful trial reported)
Autonomic Dysfunction
- Dribbling of saliva
- Trial of Atropine drops to the tongue
- Botox injections to salivary glands
- Glycopyrronium
Constipation
- Good fibre rich diet
- Laxatives – aim for combination of stimulant and osmotic
Postural Hypotension
- Increased salt and water intake
- Waist-high support stockings
- Physical counter-manoeuvres
- Avoid volume depleting drugs (diuretics, antihypertensives)
- Pharmacological therapy
- Fludrocortisone
- Midodrine
Todorova A, et al. Pract Neurol 2014;14:310–322
Curriculum Mapping
NHS Knowledge Skills Framework
- Core 2 Level 1
- HWB2 Level 1
- HWB4 Level 3
- HWB6 Level 2
- HWB7 Level 1
Foundation Programme
- Sec 1:2 Patient centred care
- Sec 1:4 Self directed learning
- Sec 3:10 Support for pts
- Sec 3:13 Discussion of medication
GPVTS
- 3.05 Communication and consultation
- 3.05 Clinical management
- Understand the management of the conditions and problems commonly associated with old age, such as Parkinson’s disease, falls, gait disorders, stroke, confusion, dementia and cancer
- 3.05 Managing medical complexity
- Understand the special features of psychiatric diseases in old age, including dementia.
Core Medical Training
- Managing long term conditions and promoting patient self-care
- Quality of life
- Natural history of disease
- Geriatric medicine Competences
- Mental state and cognitive function
- Referral for geriatric input
- Complex presentations
- Common problems: Movement disorders including Parkinson’s disease
Internal Medicine Stage 1
- Generic CIPs – Category 1:1
- Learning & teaching
- Movement disorders
Geriatric Medicine Specialty Training
- Managing long term conditions and promoting patient self-care
- Quality of life
- Natural history of disease
- 39. Movement Disorders
Physician Associate Matrix of Conditions
- 9.2.2 – Parkinson’s disease




