8.06 See and Treat at Home
Presented by: Dr Jo Preston, Dr Alice O’Connor, Dr Amy Heskett, Dr Johanna Price, Sean Edwards (Paramedic)
Contributing Faculty: Vicky Swallow (Trainee paramedic)
Special thanks to: Sabrina Vandendris (Associate Matron, Complex care support service, Croydon)
Broadcast Date: 22nd October 2019
Social media
Risk Factors and Outcomes Associated With Treatment of Asymptomatic Bacteriuria in Hospitalized Patients – Tweeted by Sean Ninan, geriatrician (@Sean9n)

https://www.ncbi.nlm.nih.gov/pubmed/31449295
Learning Outcomes
Knowledge
- To appreciate the evidence base for the benefits of both hospital and community care for older adults with frailty
Skills
- To be able to recognise those who can be managed safely at home
Attitudes
- To consider when home treatment may be a suitable option
- To involve patients in decision making regarding place of care.
Show notes
Main Discussion
Case:
Emergency Call at 09:00 on Saturday Morning, for an 89 year old woman:
She has a 3 day history of worsening fever and lethargy, with intermittent confusion. Her husband suspects a urinary infection as she has had similar symptoms with this before. This morning her carer arrived to take her to the toilet and found her weaker than usual. She had also been incontinent of urine overnight, as she was unable to get to the commode. The carer is concerned as her mobility is worse than usual and feels she will not be able to manage by herself, especially with eating and drinking.
Past medical history includes hypertension, right THR, osteoarthritis, CVA and AF.
Medications: Bisoprolol, Co-codamol, Rivaroxaban. NKDA
Social History: Carers TDS, live in own home with elderly husband, walks with frame. Has commode by bed. Non smoker and no alcohol.
O/E: Alert to voice and easily rousable. GCS 15/15. Mild fever of 38.2C
CVS – Skin pink warm and dry. Dry mucous membranes. No chest pain / dizziness / sweating / pallor. ECG shows AF with no acute changes. No postural hypotension. HS 1 + 2 + 0.
RS – Chest clear, no cough, no SOB at rest or exertion.
GI – Minimal food and fluid intake due to nausea. No D&V. Abdo soft, mild tenderness in suprapubic region. No scars / hernias / pulsatile masses.
GU – Pt is complaining of urinary frequency and incontinence, with burning on passing urine. No haematuria, no flank pain.
Urinalysis: Leu 2+, Nitrites +ve, pH 7.5. Blood trace, Ket -ve, Glucose -ve.
Neuro – FAST neg, no headache, GCS 15/15, pt has capacity. No Neuro deficit.
Mobility: Slow, but with encouragement sat on bed, then able to stand with assistance of 2 staff. Normal gait and balance, but weak and slow to mobilise. Unable to do stairs, and too weak to get up to bathroom. Rockwood Frailty score 7.
Imp: 1. LUTI, 2. Mild Dehydration
Plan: Hospital or Home?? Patient does not wish to attend ED.
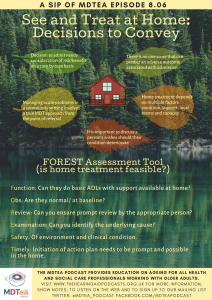
Assessment using FOREST:
For an urgent situation in a person with frailty, to consider whether home treatment is feasible (i.e. at triage)
Function: Can they do basic ADLs with care available at home/ can additional support be found?
Obs: Check in normal range or at person’s baseline.
Review: Can you ensure prompt reviews with appropriate HCP?
Examination: Needs to be thorough – can the underlying cause be identified?
Safety: Of environment and clinical condition.
Timely: Initiation of action plan needs to be prompt and possible in the home
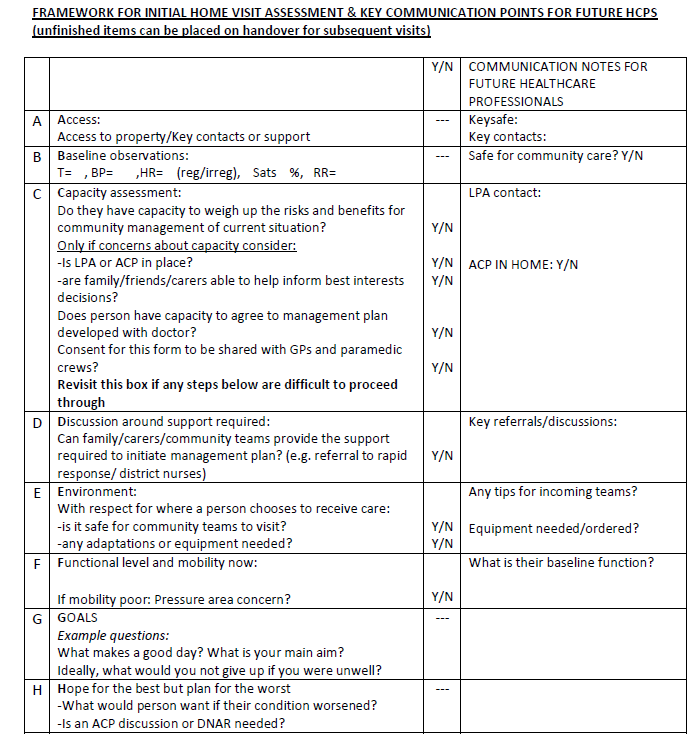
ABCDEFGH approach:
A: Access
B: Baseline observations
C: Capacity Assessment to consent to community management
D: Discussion around support required
E: Environment: safe for teams to visit? Adaptations or equipment needed?
F: Functional Level and mobility
G: Goals
H: Hope for the best, plan for the worst.
See table below, used by the Home Treatment Service in Kent:
Paramedics focus on safety net:
- Time of day e,g, middle of the day vs middle of the night
- Throughout paramedic training: focus is on acute and transfers but not with the home treatment.
- Paramedic training (specialist) in GP surgeries + hospices
SECAMB policies – built to reduce the risk of leaving someone at home but not the risks of sending someone into hospital. ‘Safest route possible’ – that adjusts with experience: is it safe, is it right? High turnover of staff means that less experienced staff are ever present.
- Using risk stratification
- Trusting the services around you
- “Your pin is on the line” approach vs being allowed to make mistakes.
- Discussion with family and patient about course of action.
- Capacity tool and best interests tool to use: widespread availability for paramedics.
Structure of a team that needs to be in place to work:
- Number of staff
- Skill mix
- Kit: e.g ABG, oxygen, iv equipment
Evidence base
No frailty score has emerged as a gold standard for measuring adverse outcomes, however some of the studies below may help clinicians and the person considering admission to weigh up the pros and cons within their current context.
Hard things to provide in a community setting:
- Care overnight
- Long term care solutions
- Not always possible to provide a quick response and those with frailty often have severe or atypical presentations requiring prompt attention
Using admission as data point is problematic as trying to “prove an admission that didn’t happen” but there are many variables which may affect this.
Effect of frailty on outcomes during hospital admission
Hubbard et al 2017 studied 1418 patients (>70 y.o.) across 11 hospitals in Australia. Frailty index scored at admission (sums person’s deficits). Score >0.4 indicates dependency on others for ADLs and a score of 0.25 indicates a person who is independent in the community. Increasing the FI by 0.1 led to a statistically significant increase in:
- LOS >28 days (OR 1.29)
- In hospital falls (OR 1.29)
- Delirium (OR 2.34)
- Pressure ulcers (OR 1.51)
- Inpatient mortality (OR 2.01)
The acute illness leading to admission may have impacted on their functional status, however this study shows that it is the current situation that is important for prognostication.
Many other studies also show this link between frailty status and adverse outcomes during inpatient stay, including the recent Hospital Frailty Risk Score in the Lancet 2018. Looked at admissions for 22,000 older people and the 20% with the highest HFRS had statistically significant increased odds of the following:
- 30 day mortality (OR 1.7)
- Long stay (OR 6.03)
- 30 day re-admission (OR 1.48)
So does this mean that hospital is bad for older adults with frailty, or is this a consequence of the severity / needs of those needing hospital, meaning that they are vulnerable to adverse outcomes? To know this, we need to know how a similar cohort of patients might do with being managed outside of the hospital environment. The immediate challenge here is having an ‘out of hospital’ set-up that is standardised and therefore comparable, which we do not. There are also many confounders beyond simply frailty scoring so, whilst it is good that we are performing more research in this area, it is difficult to produce reliable results.
This study looked at 2 cohorts:
- Ambulatory group (discharged within 72 hours, n=674)
- Inpatient group (n=246)
Frailty was estimated using 4 different scores (including Rockwood and HFRS). Depending on measure of frailty used:
32.2-36.8% of those with frailty in the ambulatory group died within the 2 year follow up
42.4-52.7% of the inpatient group died within the 2 year follow up
Those with frailty in the ambulatory group were twice as likely to die as those with no frailty. There is a high risk of poor outcomes post discharge for those with frailty and therefore there is a need for secondary prevention and links to be made with community team support.
Emergency admissions from Care Homes 2016/2017 was 7.9% of the total for those >65 years old.
41% thought to be amenable to community management. When Care Home residents are admitted as an emergency 12% die.
Cochrane Review in 2016 looked at treatments done at home that would usually require admission to hospital. 16 RCTs, n=1814, age >18 y.o. Admission avoidance schemes made little or no difference to mortality at 6 months (RR 0.77 95% CI 0.6 to .099, p=0.04). Little or no difference in likelihood of being transferred to hospital (RR 0.98 95% CI 0.77 to 1.23, p =0.84). May reduce the chance of living in RH at 6 months (RR 0.35 95% CI 0.22 to 0.57, p<0.0001). This review was only based on small RCTs and did not look at the effects on carers.
Admission Avoidance Hospital at Home. Cochrane Systematic Review. Sept 2016 Shepperd et al.
Curriculum mapping
NHS Knowledge Skills Framework
- Core 2 Level 2
- Core 3 Level 1
- Core 4 Level 1
- HWB1 Level 2
- HWB2 Level 3
- HWB5 Level 2
- HWB6 Level 3
- HWB7 Level 2
Foundation Programme
- 2. Patient centred care, Trust
- 3. Mental capacity, Protection of vulnerable groups
- 4. Self-directed learning
- 6. Communication with patients/relatives/carers, Interface with other healthcare professionals
- 9. Recognition of acute illness
- 10. The frail patient
- 11. Clinical review
- 18. Personal competence
Core Medical Training
- Time management and decision making
- The patient as central focus of care
- Team working and patient safety
- Communication with colleagues and cooperation
- Principles of medical ethics and confidentiality
- Valid consent
- Geriatric medicine: Recognise importance of multi-disciplinary assessment, Recognise the role of intermediate care, Recognise the often multi-factorial causes for clinical presentation in the elderly
GPVTS (Within Care of Older Adults)
- Making decisions
- Clinical management
- Managing medical complexity
- Working with colleagues and in teams
- Practising holistically and promoting health
- Community orientation
Geriatric Medicine Specialty Training
- Time management and decision making
- The patient as central focus of care
- Team working and patient safety
- Communication with colleagues and cooperation
- Principles of medical ethics and confidentiality
- Valid consent
- Diagnosis and management of acute illness
- Planning transfers of care including discharge
- Community practice including continuing, respite and intermediate care
- Intermediate care and community practice




