8.05 CGA in Care Homes
Presented by: Dr Jo Preston, Dr Iain Wilkinson, Jackie Lelkes, Dr Alice O’Connor
Guest: Neil Chadborn – Research fellow, PEACH study
Faculty: Dr Wendy Grosvenor
Broadcast date: 8th October 2019
Social Media
For discussion on Twitter (#MDTeaCLUB):

https://bmjopen.bmj.com/content/9/4/e026921
https://dunhillmedical.org.uk/2019/05/24/peach_blog-3c/
Learning outcomes
Knowledge
- To recall the domains of CGA in practice
- To understand the principles of integrating CGA in Care Homes
Skills
- To consider use of CGA in Care Homes
Attitudes
- To see CGA as an opportunity to tailor care in Care Homes
CPD Log
Show Notes
Definitions
Formal definition
CGA is a multidisciplinary diagnostic process intended to determine a frail elderly person’s medical, psychosocial and functional capabilities and limitations in order to develop an overall plan for treatment and long-term follow-up. Rubenstein et al (1989)
We discussed this in episode 1.1
Practical definition
A holistic assessment that leads to a plan to address issues of concern to the older person (and/ or family and carers). Interventions that follow very similar processes include case management.
Main Discussion
- The 400,000+ Care home residents in the UK are relatively high users of health care resources and may have complex needs.
- Comprehensive Geriatric Assessment (CGA) may benefit care home residents and improve efficiency of care delivery – but there is little coordinated delivery of formal CGA in care homes currently. However the recent frailty agenda may well drive a change here as the core elements of frailty assessment and care are deeply rooted in a CGA type approach.
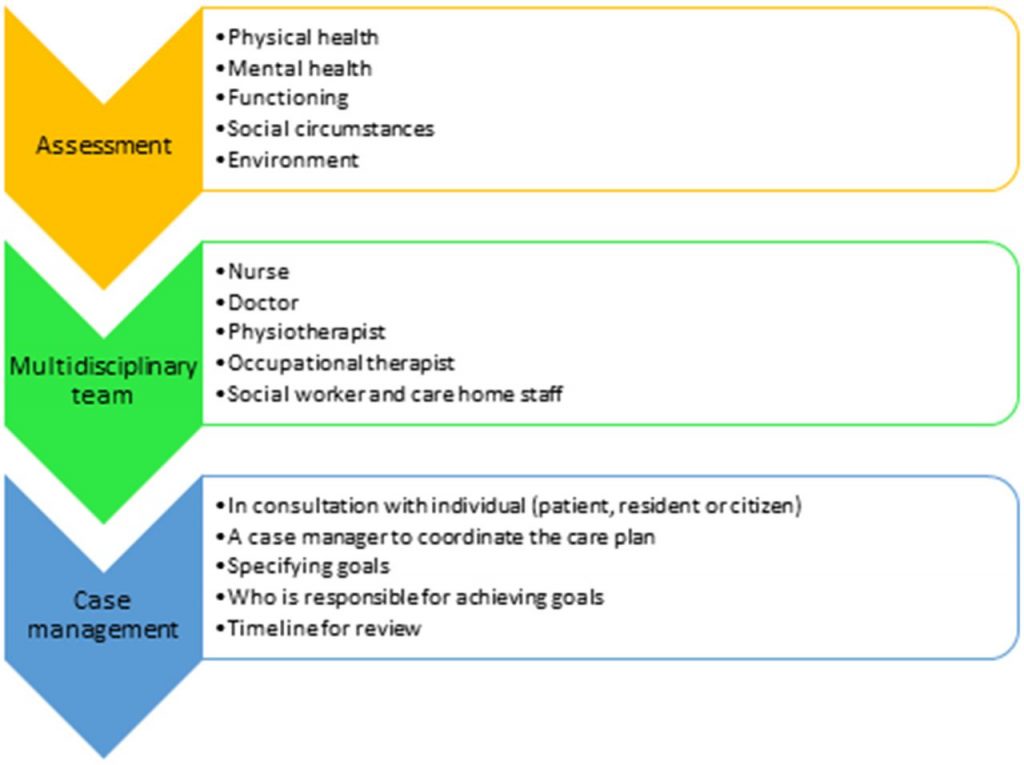
- CGA is an approach to care in which there is a thorough multidisciplinary assessment (physical and mental health, functioning, and physical and social environments, and a care plan based upon this assessment, usually delivered by a multidisciplinary team. There is often a paucity óf truly MDT care in care homes (i.e often no physio or OT support on a regular basis, and SaLT etc often involved in risk assessments more than therapy delivery).
- The CGA process is known to improve outcomes for community-dwelling older people and those in receipt of hospital care, however less is known about its efficacy in care home residents.
- Care homes are complex environments and many residents have frailty or multimorbidity. CGA is a complex intervention which may be able to improve the quality of care within care homes. However, care homes are also heterogeneous, ranging in size from a few beds to hundreds and resourced through a mix of funding models, meaning they are more complex settings than others in which to implement CGA..
- Many care home providers are private companies and have a financial agenda in addition to the care they provide.
These points develop Rubenstein’s original definition to some extent, i.e. we would like to emphasise the management (delivery of care) rather than the misinterpretation that CGA is an assessment tool. Also, more recent implementation of CGA has aimed to deliver person-centred care. This is important in the care home setting, where the MDT is more diverse and includes the primary and social care sectors, whereas the traditional CGA was developed in a hospital setting.
Components of a CGA:
Proactive Healthcare of Older People in Care Homes (PEACH) Study
The study was about Quality Improvement Collaboratives with multi-sector teams in each of 4 CCG areas of Nottingham. The aim was to implement Comprehensive Geriatric Assessment in care homes.
Study findings support the use of CGA in terms of health benefit and delivery of healthcare services. Responses from resident and family perspectives indicated a positive experience or satisfaction with services. Practitioner team members also reported positive outcomes of CGA, although for programmes that involved computerised information, care home staff identified a challenge with access to computers to enter data and read care plans, meaning that staff felt excluded from sharing views on care plans.
Summary of PEACH study Findings
- Some forms of Comprehensive Geriatric Assessment in care homes were able to change patterns of prescribing, to reduce readmission rates to hospital and to increase rates of appropriate referral to allied health professionals and palliative care teams.
- Findings of the study suggest that delivery of CGA in care homes was dependent on two contexts; how feasible it was for professionals to participate and whether the use of a structured assessment created the sense of a common purpose, challenging discipline-specific approaches and behaviours.
- They identified little description of the training or competencies required to enable CGA in a sector of health and social care where it is not routinely delivered. This made it difficult to address the feasibility of CGA in UK care homes. They recommended that further work is required to better understand the care home-specific aspects of CGA, which are essential to guide new practitioners as they attempt to implement CGA in the sector.
Recommendations:
- Teams should give careful thought to how the outputs of multidisciplinary assessment and care planning are documented and shared.
- Time needs to be set aside to agree how the priorities identified in the care plan will influence the actions of both care staff and health professionals. The findings of assessment must be both seen and actioned.
- Study found that Comprehensive Geriatric Assessment can work in care homes and that it can make a difference to resident care. Preparation and planning is required to support assessment of residents by multiple professionals, to provide a mechanism to draw the findings of assessments together, to include an appropriate mix of professionals in care planning, and to ensure the actions identified in a care plan are carried out.
Summary
CGA has three main parts:
- A structured or standardised approach to assessment
- Communication within an MDT
- Coordination of care delivery activities
- Unless all three of these components are addressed, CGA is unlikely to be successful in a care home setting.
- CGA provides an opportunity where professionals from different teams and organisations can come together with residents to establish shared priorities for healthcare: similar to the concept of ‘communicative space’.
- This has been suggested to be particularly important in care homes because they are
contested places where neither professionals nor residents may feel fully in charge of events, which may mean that implementing CGA in care homes is more complex than in other settings.
Curriculum Mapping
NHS Knowledge Skills Framework
- Core 1 Level 2
- Core 4 Level 1
- HWB2 Level 4
- HWB4 Level 2
- HWB5 Level 4
- HWB6 Level 2
- HWB7 Level 2
Foundation Programme
- 1:2. Patient centred care
- 1:4. Self-directed learning
- 2:6. Communication with patients/ relatives/ carers, Interface with other healthcare professionals.
- 2:7. Interaction with colleagues
- 3:10. The frail patient, Support for patients with long term conditions.
- 3:11. (Multiple elements within this section)
- 3:13. Discussion of medication with patients
- 3:16. Demonstrates understanding of the principles of health promotion and illness prevention
GPVTS (Within “Care of older adults”)
- CC Making decisions: recognise the importance of a problem-based approach
- CC Clinical management
- CC Managing medical complexity
- CC Working with colleagues and in teams
- CC practising holistically and promoting health
Core Medical Training
- The patient as the central focus of care
- Relationships with patients and communication within a consultation
- Communication with colleagues and cooperation
- Geriatric medicine (Multiple elements within this section)
Geriatric Medicine Specialty Training
- The patient as the central focus of care
- Managing long term conditions and promoting patient self-care
- Relationships with patients and communication within a consultation
- Communication with colleagues and cooperation
- Management and NHS structure – Understand the consistent debates and changes that occur in the NHS including the political, social, technical, economic, organisational and professional aspects that can impact on provision of service
- Evaluating performance and developing and leading services
- Comprehensive geriatric assessment
- Diagnosis and Management of Chronic Disease and Disability
- Rehabilitation and Multidisciplinary Team Working
- Community Practice Including Continuing, Respite and Intermediate Care
- Care of Older People living with Frailty




