6.06 Atrial Fibrillation
In this episode we look at the common problem of Atrial Fibrillation (the irregularly irregular heart arrhythmia).
Presented by: Dr Jo Preston, Dr Iain Wilkinson
Faculty: Dr Dan Thomas, Pam Trangmar
Broadcast Date: 16th October 2018
pdf of Sip of MDTea here
Click here for a link to the CPD log for series 6 and we’ll automatically email you a copy for your records.
Social Media
Iain:
Jo:
Top 10 books about growing old – The Guardian
Learning Objectives
Knowledge:
To understand what AF is and be able to explain this to a patient
To know why AF is a risk factor for strokes and how to reduce this risk
Skills:
To be able to detect AF by taking the pulse of a patient
To know when to refer a patient for further investigation
Attitudes:
To understand that anyone who has contact with a patient might detect AF
Show Notes
pdf here
Definitions:
Atrial fibrillation is a heart condition that causes an irregular and often abnormally fast heart rate.
Practical Definition:
Its disordered electrical activity in the atrium which leads to too many electrical impulses trying to get through the AV node. The AV node cuts many out but the result is an irregular ventricular heart beat.
Leads to an irregularly irregular pulse.
Key Points from Discussion
1. Introduction
This is the most common tachyarrhythmia in older people
- 0.5% age 50-59
- 9% age 80-89
- Risk of AF doubles with each decade of life
- in 2010 – this was 20 million men and 12 million women.
- 1 in 4 middle aged adults will develop AF
- Increases Heart failure 5x
- Cardiovascular events and all cause mortality 2x
- CKD 1.6%
- ⅓ patients who have a stroke have a diagnosis of AF made before, during or immediately after the stroke
Despite good progress in the management of patients with atrial fibrillation (AF), this arrhythmia remains one of the major causes of stroke, heart failure, sudden death, and cardiovascular morbidity in the world. Furthermore, the number of patients with AF is predicted to rise steeply in the coming years.
Increases risk of ischaemic stroke by 5-6x (but can use scoring systems to try and work out a person’s individual stroke risk) – in RCTs the stroke risk is about 1.5%.
Not only is AF a major risk factor for stroke, but when strokes occur in association with AF, patients suffer increased levels of mortality, morbidity and disability with longer hospital stays compared with stroke patients without AF .
- This is because then tend to have a large clot that will break off and block the artery (aften the middle cerebral artery) (NICE Guidance AF)
Can be
- Paroxysmal – terminates spontaneously or with intervention within 7 days
- Persistent – fails to self terminate within 7 days. often require cardioversion (can be chemical)
- Permanent – lasted more than 12 months
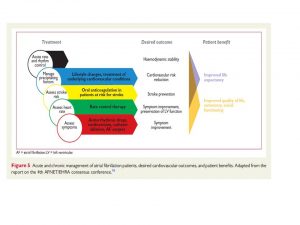
This flow chart is a good way of thinking about AF management
How to make the diagnosis?
- Manual pulse check – we can all do this! – looking for an irregularly irregular pulse
- The first person that does this when they would not normally do it and lets us know (even if its normal) will win an MDTea mug!
- We don’t this enough!!
- ECG – whenever you suspect AF
- Suspected PAF – 24 hr ECG or event recorder if symptomatic episodes are >24 hours apart
- Echocardiogram –
- for whom a baseline echocardiogram is important for long‑term management
- for whom a rhythm‑control strategy that includes cardioversion (electrical or pharmacological) is being considered
- in whom there is a high risk or a suspicion of underlying structural/functional heart disease (such as heart failure or heart murmur) that influences their subsequent management (for example, choice of antiarrhythmic drug)
Common causes
There are many of these (it’s a classic question you used to get asked at medical school)
“Give me X number of causes of AF”.
Essentially it’s anything that either leads to an unstable electrical system or a structural change to the atria – and henceforth a change to the electrical system.
- External stressors such as structural heart disease, hypertension, possibly diabetes, but also AF itself induce a slow but progressive process of structural remodelling in the atria.
- Activation of fibroblasts, enhanced connective tissue deposition, and fibrosis are the hallmarks of this process.
- In addition, atrial fatty infiltration, inflammatory infiltrates, myocyte hypertrophy, necrosis, and amyloidosis may also be found in AF patients (with their concomitant pre-disposing conditions)
- Structural remodelling results in electrical dissociation between muscle bundles and local conduction heterogeneities, favouring re-entry and perpetuation of the arrhythmia.
- In many patients, the structural remodelling process occurs before the onset of AF itself
- As some of the structural remodelling will be irreversible, early initiation of treatment seems desirable.
- The functional and structural changes in atrial myocardium and stasis of blood, especially in the left atrial appendage (LAA), generate a prothrombotic milieu
- The seminal observation by Haissaguerre et al. was that a focal source in the pulmonary veins can trigger AF, and ablation of this source can suppress recurrent AF.
Practically:
- Hypertension
- Ischaemic heart disease
- Thyrotoxicosis
- Infections
- Electrolyte abnormalities
- Alcohol
- Caffeine
- Anaemia
Symptoms – may be many, may be none!
- Palpitations
- Shortness of breath
- Light headed
- Fatigue and lethargy also common – about 15% to 20% report a decreased exercise tolerance
May need to go to hospital if
- Need urgent rate control
- Hypotension
- Heart failure
Management
- Rate + rhythm control
- Stroke prevention
Rate control – may be all you need to do to remove the symptoms – but as compared to stroke prevention and rhythm control there is relatively little evidence here.
May need emergency admission to hospital for
Management of heart failure, hypotension or difficulty controlling rate
If need initiation of antiarrhythmic drug
Treatment of associated medical problem triggering the AF e.g. pnuemonia
Can control rhythm with certain drugs, electrical cardioversion or ablation therapy
When to offer rate or rhythm control (From NICE AF 2014)
NICE guidelines say:
1.6.1 Offer rate control as the first‑line strategy to people with atrial fibrillation, except in people:
- whose atrial fibrillation has a reversible cause
- who have heart failure thought to be primarily caused by atrial fibrillation
- with new‑onset atrial fibrillation
- with atrial flutter whose condition is considered suitable for an ablation strategy to restore sinus rhythm
- for whom a rhythm control strategy would be more suitable based on clinical judgement.
- Some of the commonest drugs
- Beta blockers
- Calcium channel blockers
- Digoxin – bgs article
Anticoagulation
- There is a stroke risk with AF (can be calculated but is in the order of 4-12% per year)
- But still need to individualise risk
- To calculate stroke risk use:
- CHADS2VASC
- Heart failure
- Hypertension
- Age
- Diabetes
- Stroke
- Valvular heart disease
- Female
- CHADS2VASC
To calculate bleeding risk – HASBLED
both are here: https://www.chadsvasc.org/
Important to note that scores aren’t directly comparable i.e score of 2 on HASBLED isn’t same as score of 2 on CHADS2VASC
Also HASBLED can identify risk factors that you can modify so you could stop NSAIDS or Aspirin, control hypertension and reduce alcohol intake to lower the bleeding risk
Can use SPARCTOOL.com (can download to phone) will compare the HASBLED and CHADS2VASC and give a Number needed to treat and Number needed to harm of Warfarin, Apixaban, Rivaroxiban, Edoxaban, Dabigatran
- Commonly see falls as a reason why people in AF aren’t anticoagulated
- ‘Choosing antithrombotic therapy for elderly patients with AF at risk of falls’
- 295 falls in one year before risk of bleeding outweighs stroke risk if in AF on Warfarin and over age 75 (according to one study)
Commentary in Journal Watch October 2012 here
- Still see people on Aspirin or Clopidogrel for AF (No longer recommended as per most recent NICE guidance as did not prevent strokes cause by AF but did carry risk of bleeding)
- Why not Aspirin?
- No benefit in all cause mortality, ischaemic stroke, systemic emboli or reducing major bleed
What if Warfarin control of poor? (consider DOAC) if:
- TTR of 65% or less
- 1 INR above 8
- 2 INR above 5
- 2 INR less than 1.5
- But can be useful if people don’t want frequent blood tests, have difficulty getting to GP surgery or anticoagulation clinic
Advantages and Disadvantages to various DOACS each is really an individual decision to be taken with the patient.
Curriculum Mapping
| Curriculum | Area |
| NHS Knowledge Skills Framework | Suitable to support staff at the following levels:
|
| Foundation curriculum | 2. Delivers patient centred care and maintains trust
9. Recognises, assesses and initiates management of the acutely ill patient 10. Recognises, assesses and manages patients with long term conditions 12. Requests relevant investigations and acts upon results |
| Physician Associate Matrix of Conditions | Atrial Fibrillation
Stroke |
| Core Medical Training | The patient as central focus of care
Palpitations Therapeutics and safe prescribing Decision making and clinical reasoning Managing long term conditions and promoting patient self-care Evidence and guidelines |
| GPVTS program | 3.12 – Cardiovascular health, AF
3.05 – Care of Older Adults – stroke |
| ANP (Draws from KSF) | 7.5 Stroke and cerebrovascular disease
7.7 Atrial fibrillation |
| Geriatric Medicine – Higher Specialist Training | 3.2.3 Presentations of Other Illnesses in Older Persons
3.2.9 Health Promotion – Risk reduction for stroke 28. Diagnosis and Management of Acute Illness 29. Diagnosis and Management of Chronic Disease and Disability |





1 Response
[…] S6E6 – Atrial Fibrillation […]