5.08 Hearing
Episode 5.08 Hearing
Presented by: Dr Jo Preston, Dr Iain Wilkinson, Kerry James Clark
Faculty: Owen Ingram
Broadcast Date: 15th May 2018
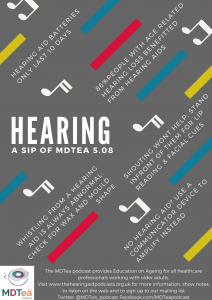
Click here for a pdf of the sip of MDTea poster
Click here for a pdf of show notes
CPD log
Click here to log your CPD online and receive a copy by email.
Tweetchat #MDTeaClub
We will be hosting a ‘journal club’ type tweet chat to discuss topics raised in this episode using #MDTeaClub
Join us to discuss topics raised in the episode and spread any resources you may have!
Social Media this week
Iain’s choice: Evergreen Olympics in Thailand for those middle aged and above. Promoting wellbeing and activity by the government.
Jo’s choice: Free induction booklet for those rotating into placements working with older adults by @COTEBangor – they make a lot of other great infographics that are free to use and share too.
Pssst! Junior docs… if you’ve rotated to a job with lots of geriatric patients (which is most jobs except paeds & obstetrics…) and are feeling a bit daunted, we can help. Download our “Top Tops for COTE beginners” e-booklet from https://t.co/OSpzgdq75F #FOAMed pic.twitter.com/VfKuOnee0h
— COTE Bangor (@COTEBangor) 7 February 2018
Main Show Notes:
Learning Outcomes
Knowledge:
- Understand the association between hearing impairment, cognitive impairment and low mood
Skills:
- Know how to troubleshoot common problems with hearing aid.
Attitudes:
- Appreciate the impact of hearing loss on quality of life.
Definitions:
Hearing is an old Middle English word from the 1170s, meaning:
The faculty or sense by which sound is perceived or the act of perceiving sound.
That is, the neurological representation of a sound.
Key Points from Discussion
Epidemiology:
- Hearing loss in adults is a common and important problem
- 4th leading cause of disability globally
- Prevalence doubles with every 10 year increase in age
- 50% of 60 year olds
- 2/3rds over 70s
- 85% of over 85 year olds
- An ageing population will lead to an ever increasing absolute number of people with hearing loss
Cunnigham et. al. Hearing Loss in Adults. N Engl J Med 2017
Frank R. Lin et. al. Hearing Loss Prevalence and Risk Factors Among Older Adults in the United States, The Journals of Gerontology: Series A 2011
Why is it important?
Hearing loss is common but usually benign and not a dangerous symptom
- It can however adversely affect communication if left untreated which leads to increased levels of social isolation, mood disorders and there is an association with increased rates of cognitive impairment
- It is often left undiagnosed but management is easily accessible and very effective
Red Flags – for when hearing loss could be a sign of something needing medical assessment:
- Sudden onset symptoms – which can be a sign of ‘sudden neural hearing loss – an audiological emergency often requiring urgent steroids (under ENT or Audiovestibular Physician)
- Unilateral symptoms
- Conductive hearing loss (that is not wax impaction)
- Associated ear symptoms:
- Otalgia – pain in the ear
- Otorrhoea – discharge from the ear
- Abnormal ear drum
- Associated neurological symptoms:
- Balance disorder
- Vertigo
- Unilateral / pulsatile tinnitus
Fook L, Morgan R. Hearing impairment in older people: a review. Postgraduate Medical Journal 2000
Quick anatomy of the ear to understand the processes that cause hearing loss:
It is important to have a basic understanding of the anatomy because our bedside assessments can guide us to what is causing a specific hearing loss.
Damage or disease in the outer or middle ear will cause conductive deafness whereas damage to the inner ear and neural pathway to the brain will cause sensorineural deafness and the two different diagnoses require different approaches to investigation and management.
The ear itself anatomically is split into 3 parts; all 3 parts need to be functioning well as does the nerve connecting the ear to the brain and the brain itself.
- Outer ear: made up of the pinna and the external auditory canal and ends at the tympanic membrane (eardrum)
- The External auditory canal is commonly blocked with wax – wax impaction
- Very common problem affecting the outer ear
- Treated with olive oil ear drops 2 drops twice a day, followed by ear irrigation and sometimes microsuction.
- The External auditory canal is commonly blocked with wax – wax impaction
- Middle ear: made up of the tympanic membrane and ossicles – 3 small bones connecting the eardrum to the cochlear
- The eardrum can be damaged by pressure changes, trauma or infection of the middle ear – otitis media ; painful / discharge / post URTI / fever
- The bones can become fixed – otosclerosis; progressive hearing loss
- Inner ear: made up of the specialist hearing apparatus the cochlear and the semicircular canals
- The cochlear is a small circular organ which in shape looks like the shell of a snail – it collects the sounds from the ear and converts them to electrical signals to send to the brain
- It can be damaged by drugs, noise and ageing
- The semicircular canals are 3 tubular arches which sit in different planes, they are vital in balance
- We won’t be talking specifically about balance disorders today
Meniere’s disease is a disease of the inner ear
-
- Characterised by episodic vertigo, tinnitus and hearing loss (20 mins to a few hours)
- Thought to be caused by a change in the fluid build up in the inner ear
- Be sure to rule out acoustic neuroma
- Treatment is with information and guidance on the illness and symptoms expected plus as required vestibular sedatives for dizziness
The neural pathway and acoustic neuroma
The 8th cranial nerve, the vestibulocochlear nerve, links the cochlea to the cortex of the brain and damage to the nerve will cause sensorineural hearing loss as well as damage to the cortex of the brain. Acoustic neuroma is a common cause of ‘central’ hearing loss – damage to the brain causing hearing loss. It is a tumour of the vestibulocochlear nerve and can cause pressure on brain structures near the nerve.
Presents with unilateral sensorineural hearing loss and can be associated with cerebellar signs and other cranial nerve signs which should be examined as part of a hearing assessment:
- Balance and gait disorder
- Nystagmus
- Dysdiadokinesis
- Facial weakness
Often requires surgical treatment but many require watchful waiting – particularly older people. Monitored with imaging and audiometric testing. Radiosurgery is another option (stereotactic radiotherapy / gamma knife)
Changes in hearing with ageing
By far the commonest type of hearing loss you are likely to encounter in the elderly is Age-related hearing loss or ‘presbycusis’.
Age related hearing loss is:
- Sensorineural
- Slowly progressive
- Bilateral
- Classically lose higher pitched sounds
- Find it difficult to understand speech
It is characterised by:
- Degeneration of the sensory hair cells in the cochlear
- Degeneration of the nerve cells that send sensory inputs to the brain
- Atrophy of the stria vascularis (membrane of cochlear that makes endolymph)
Causes include:
- Genetic predisposition – Age related hearing loss runs in families
- Accumulation of other stressors to the cochlear:
- Noise exposure
- Specific drugs:
- Gentamicin / aminoglycosides – 20% incidence of hearing loss
- Cisplatin – 60% incidence of hearing loss. A chemotherapy used for testicular cancer and haematological malignancies
How to approach a patient presenting with hearing loss and identifying the red flags:
History
- Bilateral (Presbycusis, wax) vs unilateral (Acoustic neuroma, wax, otitis media, perforated eardrum)
- Time of onset; sudden (perforated eardrum), days, weeks or months (wax, presbycusis, acoustic neuroma)
- Associated symptoms: Otalgia and Otorrhea (otitis media / perforated eardrum), vertigo and tinnitus (Meniere’s / central cause of hearing loss)
- Exposure to ototoxic drugs?
- Occupation
- Family history
Examination tips
- Inspect the outer ear:
- Looks for vesicles (Ramsay hunt), erythema (Otitis externa), otorrhea
- Otoscopy
- Look for wax
- Visualise the eardrum – confirm intact, translucent and glistening
- Forced whisper test
- Good screening test
- Stand at arm’s length away
- Whisper a combination of 3 letters and numbers
- Test each ear individually
Pirozzo et al. Whispered voice test for screening for hearing impairment in adults and children: systematic review. BMJ 2003
- Rinne and Webers test
- Checks for conductive vs sensorineural
- Extra tests to consider:
- Balance and gait
- Nystagmus
- Dysdiadokinesis
- Facial weakness
For those over 60, if the hearing impairment appears to be progressive, bilateral and sensorineural in origin – with normal ear examination; GPs and hospital clinicians should diagnose age related hearing loss and make a direct referral to hospital audiology departments.
Audiology Assessment:
Screening is not routine as per visual problems
- This is because many people with mild hearing loss are not significantly affected by hearing aids
- Also many people are not ready to start wearing hearing aids
Usually assessment is carried out at the local audiology department – usually a long wait for this. Some other options
- Call: 0845 600 55 55 for a phone hearing test
- http://www.mabels.org.uk/hearing-phone-test.php
- Pharmacies / opticians often offer free hearing tests
- Age UK and hidden hearing can help arrange home visits for hearing tests:
- There is an on-line hearing test from Action on Hearing Loss
Management of age related hearing loss:
- Hearing aids – choice related to aesthetics and eased of use
- 86% of patients benefited from hearing aid correction with age related hearing loss
- 14% of people with hearing loss reported wearing hearing aids
Cunnigham et. al. Hearing Loss in Adults. N Engl J Med 2017
Abdellaoui et al. Success and failure factors for hearing-aid prescription: Results of a French national survey. European annals of otorhinolaryngology, head and neck diseases, 2013
Hearing Aids on the NHS – what to know
- Hearing aids are available on the NHS for anyone who needs one
- Batteries and repairs are free
- Assessment and after care is free
- Generally only behind the ear versions
- Waiting time longer than for private treatment
- Privately can cost £500-£3500 per hearing aid
Types available
- Behind the ear hearing aids (BTE)
- Most common – only one available on NHS
- Completely in the canal hearing aids
- Smaller still
- Need to be fitted by hearing aid technician
- Often aren’t powerful enough
- Receiver in the ear hearing aids
- Less visible that BTE
- More fiddly to use
- In the canal hearing aids
- Similar to in the ear, but significantly smaller
- BAHA – Bone Conducting Implant – Good for Conductive hearing loss / Mixed hearing loss
- Cochlear implants
-
- Used for people with severe or total sensorineural hearing loss
- Only allowed 1
- Implanted to bypass the patients cochlear and directly stimulate the cochlear nerve
- Not regularly used in the elderly – requires GA, 3 hour operation
- Cost £40K privately
- 2 weekly f/u for 3/12 post procedure
- Has been shown to be safe and increase quality of life in the elderly population and may improve cognitive impairment – so should be considered more often – are being used now more commonly in the older cohort of patient.
Mosnier et al. Improvement of Cognitive Function After Cochlear Implantation in Elderly Patients. JAMA Otolaryngol Head Neck Surg. 2015
NICE Health Technology Appraisal. Cochlear Implants for Deafness in Children and Adults. March 2007
Hearing Therapy
- In addition to hearing aids, audiology departments offer hearing therapy – an important benefit of the NHS
- This is important for associated symptoms e.g tinnitus
- It is also important for counselling pre using hearing aids which is often very important
Advice to given the patient when starting to use a hearing aid / troubleshooting:
- Normally switched on by pushing battery clip in – older ones have an on and off button
- There is a separate button for the telecoil mode (pick up signals from loop devices and telephones – found in buses, banks and theatres) – many don’t work
- It takes at least 6 weeks for the hearing aid to work – reprogramming of neural pathways so persist (acclimatisation period)
- Explain that the aid will amplify the sound – but will not normalise your hearing
- Whistling is always abnormal: could be sign of wax or ill-fitting hearing aid
- No sound / muffled sound:
- Check its switched on
- Check the volume is up
- Check you are not on the telecoil setting
- Check the tubing isn’t blocked with wax
- Check the battery is in the right way round
- Get a new battery
Action on Hearing Loss: Life with Hearing Aids Leaflet
- Hearing aid batteries have a short life span (approx. 10 days)
- Here’s a video on how to unblock a hearing aid
Assisted Listening Devices (ALD)
- Equipment around the home to aid hearing:
- Loop system for the TV
- Microphones
- Smoke alarms (fitted by fire service normally)
- Flashing doorbells
- Fire service offer a free safety check
- Veterans Support Charity offer much equipment ALDs and support for veterans with hearing loss
Tips for the ward / clinic environment for people with untreated hearing loss:
- Recent study showed 43% of patients had misheard a healthcare professional in their recent attendance to hospital
Cudmore et al. Age-Related Hearing Loss and Communication Breakdown in the Clinical Setting. JAMA Otolaryngol Head Neck Surg. 2017
- Try to get access to a communicator from your audiology department (Approx £50 – could be available on all wards for a small price)
- Don’t just shout as the intonation in your voice changes making it harder to hear
- Pick the side with the better ear
- Remember that most patients with hearing loss rely on lip-reading so be clear with your facial expression
- Consider using a whiteboard to aid communication
- Don’t end up talking to patient’s relatives because it is easier – make sure you work hard to talk to the patient.
Consequences of hearing loss in the elderly:
- Cognitive decline
- Hearing loss is associated with cognitive decline
- This may in part be due to common aetiologies – vascular risk factors
- Those with moderate hearing loss score lower in non-verbal reasoning tests than those with normal hearing
- Those with cognitive decline have more accelerated decline if moderate hearing loss is left untreated
- Use of hearing aids has been shown to improve performance of cognitive tests
- With return to baseline on stopping hearing aid use
- Hearing loss is associated with cognitive decline
- The current evidence suggest that:
- Age-related hearing loss is a possible biomarker and modifiable risk factor for cognitive decline, cognitive impairment, and dementia.
- Additional research and randomized clinical trials are warranted to examine implications of treatment for cognition
Loughrey et al. Association of Age-Related Hearing Loss With Cognitive Function, Cognitive Impairment, and Dementia A Systematic Review and Meta-analysis. JAMA Otolaryngol Head Neck Surg 2017
Hewitt D. Age-Related Hearing Loss and Cognitive Decline: You Haven’t Heard the Half of It. Front. Aging Neurosci. 2017
- Depression, anxiety and social isolation
- In an American Study – National Council on the Aging
- Higher rates of sadness and depression and worry and anxiety in older patients with hearing impairment compared to those who use hearing aids
- Higher rates of social isolation
- Hearing aid users reported significant improvement in quality of life since using hearing aids, specific improvements in:
- In an American Study – National Council on the Aging
| Improvement Area | Improvement Reported by Hearing Aid User (%) | Improvement Reported by User’s Family (%) |
| Relations at home | 56 | 66 |
| Feelings about self | 50 | 60 |
| Life overall | 48 | 62 |
| Relations with children, grandchildren | 40 | 52 |
| Mental health | 36 | 39 |
| Self-confidence | 39 | 46 |
| Sense of safety | 34 | 37 |
| Social life | 34 | 41 |
| Relations at work | 26 | 43 |
| Sex life | 8 | NA |
The National Council on the Aging; The Consequences of Untreated Hearing Loss in Older Persons. May 1999
Curriculum Mapping:
This episode covers the following areas (n.b not all areas are covered in detail in this single episode):
| Curriculum | Area | |
| Higher Specialist Training Geriatric Medicine | Diagnosis and Management of Chronic Disease and Disability | |
| NHS Knowledge Skills Framework | Suitable to support staff at the following levels:
Equipment and devices to meet health and wellbeing needs: Level 1-2 | |
| Foundation curriculum | Section
2.6 3.1
3.16 | Title
Communicates clearly in a variety of settings Recognises, assesses and manages patients with long term conditions Demonstrates understanding of the principles of health promotion and illness prevention |
| Core Medical Training | Managing Long Term Conditions and Promoting patient self-care
Relationships with patients and communication within a consultation | |
| GPVTS program | Section 3.15 Care of people with ENT, oral and facial problems
Section 3.05 – Managing older adults
| |
| ANP (Draws from KSF) | 7.29 Vision and hearing problems. |