4.06 Vision
Presented by:
Dr Iain Wilkinson (Consultant Geriatrician East Surrey Hospital)
Dr Jo Preston (Consultant Geriatrician St George’s Hospital)
Faculty:
Dr Neruban Kumaran, Ophthalmology Registrar, Moorfields Eye Hospital
Dr Gabor Szekely, General Practitioner
Sip of MDTea
PDF version of this infographic here
Broadcast date: 24th October 2017
CPD log
Click here to log your CPD online and receive a copy by email.
Tweetchat #MDTeaClub
We will be hosting a ‘journal club’ type tweet chat to discuss topics raised in the episode on 1st November at 8.30pm GMT using #MDTeaClub
Join us to discuss topics raised in the episode.
Social Media Spots This Week
The Use of Storytelling in Medicine https://t.co/eXCRLyU24o pic.twitter.com/9TUIOVqDpI
— JAMAInternalMed (@JAMAInternalMed) October 20, 2017
.@NIHR_DC Signal ft. @CochraneEPOC evidence “Nurses and pharmacists can prescribe as effectively as doctors”https://t.co/PaUhuHpuwK
— Cochrane UK (@CochraneUK) May 21, 2017
Show notes (PDF here)
Learning Outcomes
Knowledge:
- To recall the common causes of visual loss in older adults
- To know how these are managed
Skills:
- To be able to undertake an initial history about visual loss
- To recognise when onward referral is beneficial
Attitudes:
- To appreciate that visual loss can be a modifiable condition
- To consider visual assessment in those falling, with delirium and as part of a CGA.
Definitions:
Vision can be measured and defined in many different ways e.g. central or peripheral acuity, and more subtle elements such as contrast and colour. All of which contribute to ability to see and perceive the world. In practice al forms used day to day but not all of them can be tested and quantified for routine testing but many can.
Practical Definition:
Practically, visual testing in an ophthalmology clinic with take into account more of these items than just acuity but will also focus testing on the relevant area of difficulty or in relation to their problem.
Blind is a term moving away from, instead: severely visually impaired or partially sighted. Generally everyone should be seen by an ophthalmologist to assess and diagnose blindness because
- Assess more than central acuity (e.g. Snellen chart), to get better picture
- Inform GP so can access additional services
- Royal College Ophthalmology data for epidemiological surveillance
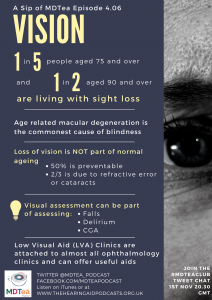
- Low Visual Aid (LVA) Clinic attached to almost all ophthalmology clinics
- Charitably supported
- Ensure all available useful aids are offered
- Links to social services too
Key Points from Discussion
Sight loss affects people of all ages, but as we get older we are increasingly likely to experience sight loss.
- One in five people aged 75 and over are living with sight loss.
- One in two people aged 90 and over are living with sight loss.
- Nearly two-thirds of people living with sight loss are women.
- People from black and minority ethnic communities are at greater risk of some of the leading causes of sight loss.
- Adults with learning disabilities are 10 times more likely to be blind or partially sighted than the general population.
Causes of visual loss
- Age related macular degeneration is commonest cause of blindness
- Other significant causes include cataract, glaucoma and diabetic retinopathy
Red Flag features that need medical or ophthalmological review
- Curtain across visual field: amaurosis fugax and retinal detachment
- Part of visual field e.g. just one side: may be neurological
- Painful red eye (except if confident it is simple viral conjunctivitis -> chloramphenicol)
- Associated headache, nausea and vomiting (with red eye): acute angle closure glaucoma
- Orbital cellulitis – i.e. near or around the eye, high risk for tracking backwards
Is it part and parcel of Ageing?
- 50% is preventable
- ⅔ of visual loss is due to refractive error or cataracts
- NB accommodation (reading) reduces after age of 40
RNIB Evidence Based Review: People in Later Life
There is a link between sight loss and reduced wellbeing. Over one-third of older people with sight loss are also living with depression.
Hodge, Barr and Knox (2010) Evaluation of emotional support
When should you check vision?
- As part of a falls assessment
- Delirium
- CGA
Vision is a big modifiable risk factor for falls. Remember varifocals are a risk factor, however changing type of varifocal lens can also make someone more likely to fall.
Age Related Macular Degeneration: Wet and Dry
- Both cause painless distortion of vision in one eye: Straight to squiggly lines.
- WET: onset over days – urgent referral
- Treatment should start within 2 weeks
- Eye injections with local anaesthetic at first assessment
- Once a month for 3 months, then PRN (clinic monitoring usually)
- DRY: onset gradual over years – supportive management
- Fish oils and green vegetables may help slow progression
- Central loss of visual acuity, usually complain of worsening vision, thinking need new glasses.
Cataracts
- Complain of glare, particularly at night / when driving in low light.
- Gradual onset
- Almost always operable
- Local anaesthetic
- Lie flat and still 30 mins
- Home same day
- One eye at a time: risk of infection (1 in 1000)
Glaucoma (Open Angle or ‘Chronic’)
- Raised pressure in eye due to flow problems with circulation of fluid in the front of the eye (the aqueous humour), anterior chamber: in front of iris.
- Peripheral visual field loss
- Often asymptomatic otherwise
- More common in afro caribbean descent, short sighted and those with family history
- Free eye tests for >40 if first degree relative
- Drops mainstay of treatment to improve drainage of eye
- Changes in pressure are main issue so avoid missing doses
- Drops:
- prostaglandin analogue
- beta-blocker (note these can be absorbed systemically as administration to eye avoids 1st pass metabolism)
- carbonic anhydrase
Non-visual eye problems
Dry eyes
- Common, benign condition with potentially high symptom burden
- Lubricating drops to increase protective liquid layer over eye
- Chronic blepharitis common cause
- Glands at base of eye lashes produce oils, help stop tears evaporating
- Can get blocked by dry skin: good eye lash care can help keep glands open
Entropion and Ectropion
- Eyelids curving in or out of lower due to lid laxity
- Drops to maintain protective layer over eye
- Uncomfortable but usually benign, can use tape to keep eye lid out
- Operation if needed.
Eye drop administration tips
1 drop = 1 dose
If someone has two types of drops, wait 5 minutes between administration
How to administer eye drops as described by Neruban
Access
Community optometrist can do a lot of initial assessment in say NH or at home if unable to get to clinic.
High street optician will have more equipment to do fuller assessment e.g. check pressures, visual fields, look at retina, check for cataracts, refractive errors. Particularly acuity: are they wearing the right glasses?
Eye tests are free for over 60s.
Care Home Residents
UK based study looking at barriers to access included limited awareness of eye health and eye disease, concern about the cost of spectacles and the appropriateness of optometry in a commercial setting. Attendance at the optometrist was primarily symptom led. A positive previous experience or continuing relationship with the optometrist helped to alleviate the barriers and promote attendance.
Improving access to optometry services for people at risk of preventable sight loss: a qualitative study in five UK locations. Leamon et. al Journal of Public Health 2014
Good eye health contribute to a lower rate of falls, depression and isolation; and better quality of life.
Undetected sight loss in care homes: an evidence review July 2012 by ILCUK
Ask the Ophthalmologist – your questions from Twitter
Q: ?Value (and how) of contrast sensitivity testing on inpatients for falls prevention. (Gareth Clifford @gcliffordpt)
A: Although extremely valuable, contrast sensitivity is not routinely tested in a clinic setting. This is a very important aspect of vision and important to be aware of, as there are adaptations for reduced contrast sensitivity such as contrasting door knobs and toilet seats.
Q: How to do bedside assessment of 3d vision and evidence for changes in 3d vision in pt with Parkinson’s (Jo Jennings @JoJenningsNHS)
A: In practice if you have good vision in both eyes you are likely to have an element of stereopsis (depth perception). This can be tested in the ophthalmology department. If you have a worry about stereopsis, discuss with ophthalmology.
Q: If you suspect acute glaucoma (esp if some distance or delay from eye centre) should you treat before sending for Ax and if so with what? (Sandy Thomson @DrSandyThomson)
A: If worried about acute glaucoma, get in touch with the Opthalmologist as there are many differentials for raised intraocular pressure- they need to be seen and assessed promptly. Wouldn’t recommend giving treatment before assessment.
Resources
http://www.dlf.org.uk/factsheets/vision
Curriculum Mapping:
This episode covers the following areas (n.b not all areas are covered in detail in this single episode):
| NHS Knowledge Skills Framework | Suitable to support staff at the following levels:
| |
| Foundation curriculum | Section
3.11 3.16 | |
| Core Medical Training | Common Competences:
System specific competences
| |
| GPVTS program | Section 3.05 – Managing older adults
Section 3.16 Care of people with eye problems | |
| ANP (Draws from KSF) | Section | |
| Physician Associate Matrix of conditions | Section 6 – Eye |