11.6 A Day in the Life of a Physiotherapist
Presented by: Iain Wilkinson, Stephen Collins and Georgie Gill
Contributors: Amy Lamacraft, Joe Middleton, Grace McVicar and Ailie Rodgers
Broadcast date: 22 march 2022
Learning Outcomes:
Knowledge:
- To know what physiotherapists main priorities are in patient assessment and care.
- To know the range of skills physiotherapists may employ in patient care
Skills:
- To be able to identify patients who may benefit from physiotherapy input
Attitudes:
- To understand the value of therapy teams within the MDTea.
Social Media this week
Iain spoke about a tweet from Alistair MacLullich and a paper the was published as part of the DELINEATE Study and talks about the impact of delirium in ED.
Delirium in the ED frequently persists into hospitalisation, and longer periods of delirium in ED are associated with worsened functional and cognitive outcomes at 6 months.
Early detection of #delirium including in the ED is crucial.@RCEMevents #RCEMdel@WesElyMD @JinHanMD pic.twitter.com/dH9nyOi7nP
— Alasdair MacLullich (@A_MacLullich) March 1, 2022
Stephen spoke about the Planning Ahead tool that Katherine Mannix kindly tweeted us about. We’ve had a look and were really impressed at the design and ease of use to assist patients and families discussion about priorities and wishes for care in the later stages of life. It’s a trial site at the moment.
You can see the site here: Planning Ahead
Main show notes
Physiotherapists in the Emergency Department can have a role in the assessment and discharge of patients.
Therapists like Amy may see the patient tracker or hear handover from ambulance crews bringing patients in to begin the social assessment early. This way they are making the best use of the 4 hour window thats patients ED care should take, to get social assessments complete, so that when they need to assess movement they’re ready.
Front door Frailty is a rapidly developing area of healthcare in the UK as the population of older adults rises.
We covered Front Door Frailty in series 7 episode 5- Have a listen here.
The NHS Long term plan talks about the Aging Well and emphasises the role of a multi professional team that includes doctors, nurses and allied health professionals all working together to support people to live well, at home for longer.
We talked about how whilst Physiotherapists and Occupational Therapists do work very closely together within therapy teams they are different professionals with differing priorities and approaches to patient care. Grace spoke about how useful joint assessments with OT and Physio can be during her work.
In the hospital Physios are not looking at joint specific movement, instead they’re looking at ensuring patients have safe and effective transfers and movement e.g getting out of bed, transferring to a chair and walking.
OT’s meanwhile are looking at supporting patients to complete activities of daily living.
Physiotherapists have a key role in supporting and making decisions about patient discharge. We talked about how they perhaps mark the change from a medical model of assessment and care of patients to utilising a more social and holistic model.
We asked the physios to think of ways we as an MDT can help support their work and they had a few suggestions.
- – Proactive pain management
- – Gathering detailed collateral history
- – Empowering patient choice over their care
- – Supporting and designing services that empower patient choice
We spoke with Ailie a respiratory Physiotherapist currently working in a surgical unit. She told us about how respiratory physiotherapists are available on call 24/7 365 days a year.
She spoke about the role of the physio in supporting patients with use of cough assist devices, suction and breathing exercises. As an MDT having an awareness of the huge range of skills a physiotherapist might have can really help us make sure we are using them to maximum benefit.
All clinicians working in the MDT have a role to support patients to maintain their level of movement and function.
Not all patients need to see a physiotherapist during an admission.
Physiotherapists are not a ‘get out of bed’ service, and it is important that we as a team feel confident in supporting patients to get out of bed, sit in chairs and mobilise effectively during an admission. Nursing staff can play a key role in supporting patients daily movement.
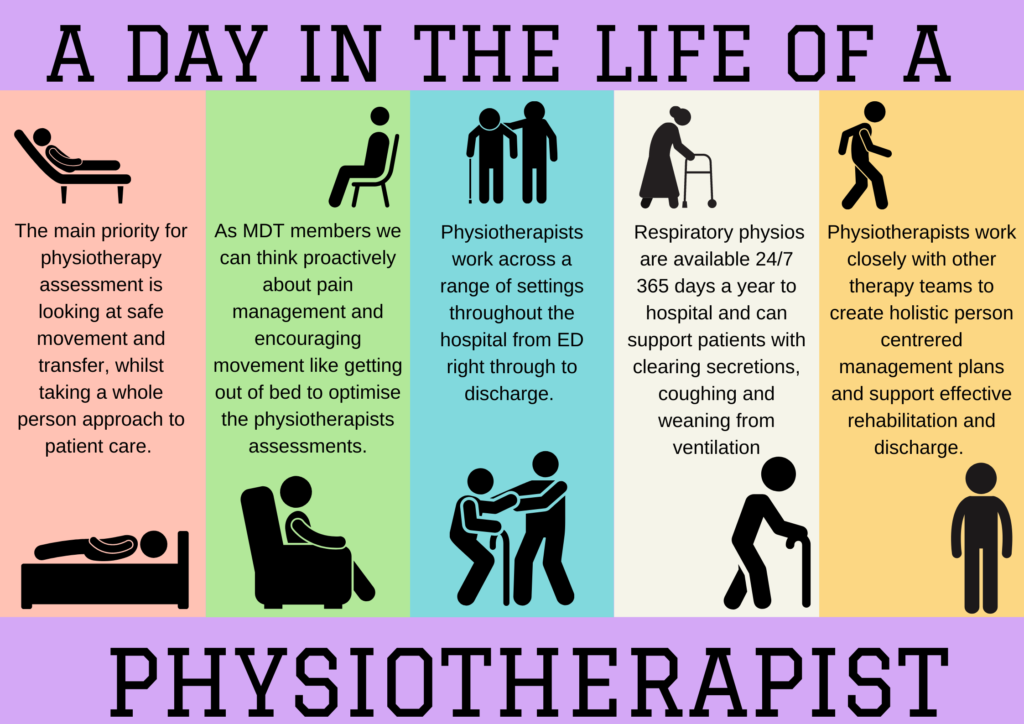
Key learning points from ‘A day in the life of a Physiotherapist’
1) The main priorities for physio assessment is looking at safe movement and safe transfer, whilst taking a whole person approach to patient care.
2) As an MDT member we can think proactively about pain management and encouraging movement like getting out of bed to optimise the physiotherapists assessments.
3) That physios work across a range of settings throughout the hospital from ED right through to discharge.
4) Respiratory physios are available 24/7 365 days a year to hospital and can support patients with clearing secretions, coughing and weaning from ventilation. They work with older adults in surgical wards, respiratory wards and ITU.
5) Physios are not just a get out of bed service and we can work together within the MDT to create a holistic person centred management plan.
How are physiotherpaists involved in caring for Jean?
Jean might be seen by a number of physiotherapists during her time at the hospital.
First she might be seen in the Emergency department by someone like Joe or Amy.They would assess Jeans pain, gather a social history and assess her mobility in the department. They might assess her mobility and find she is below her baseline and along with the chest x-ray and unknown cause of fall, they might suggest she needs admission to a ward.

Jean might meet a physiotherapist on the ward, and on her first day staying in the ward she’d be a priority one for physiotherpists the meet her and review her needs.
They would want to time their assessments with her parkinsons medications in order to optimise Jeans movement quality during assessment. They’d also likley chat to Jeans son to gether a bit more social history about Jean such as what her house is like, does she have stairs, does she use mobility aids, what daily tasks does she do herself, whats her cognition like day to day?
The therapy teams would also assess Jeans cognition during assessment whilst assessing her movement. They’d assess transfers such as getting in and out of bed, working to make the environment as similar to their home as possible- such as flattening the bed, or using stairs.
Curriculum mapping
NHS key skills framework
Core:
Communication 2
Communicate with a range of people on a range of matters
HWB4:
L2 Enable people to meet ongoing health and wellbeing needs.
L3 Plan , deliver and evaluate care to meet peoples health and wellbeing needs
Foundation Curriculum
FY1
2.6
Describes the structure and importance of the wider healthcare team.
Works effectively within the healthcare team for the benefit of patient care.
Makes clear, concise and timely written and oral referrals to other healthcare professionals within the hospital.
2.7
Acts as a member of the multidisciplinary professional team by supporting, respecting and being receptive to the views of other healthcare professionals.
Works effectively with others towards a common goal e.g. accepts instructions and allocation of tasks from seniors at handovers and multidisciplinary team meetings.
4:20
Demonstrates understanding of the organisational structure of the NHS and independent sector and their role in the wider health and social care landscape.
Describes hospital and departmental management structure.
FY2
2.7: Interaction with Colleagues
Demonstrates initiative e.g. by recognising work pressures on others, providing support and organising / allocating work to optimise effectiveness within the clinical team
GP Training Curriculum
Clinical management:
Contribute to an organisational and professional approach that facilitates continuity of care (e.g. through adequate record keeping and building long term patient relationships)
Organise follow up of your patients after referral through multiprofessional, team bases and structured approaches including monitoring, reviewing and regular care planning.
Working with colleagues and in teams:
Enhance working relationships by demonstrating understanding, giving effective feedback and maintaining trust.
Appropriately seek advice from other professionals and team members according to their roles and expertise.
Core Medical Training curriculum
Define the role of rehabilitation services and the multi-disciplinary team to facilitate long-term care
Internal Medicine Training Curriculum
2.3:
Communicates effectively and is able to share decision making, while maintaining appropriate situational awareness, professional behaviour and professional judgement
Geriatrics and higher specialty training curriculum
27:
Have knowledge of the range of agencies that can provide care and support both in and out of hospital and how they can be accessed
30:
Rehab and MDT working. Roles and expertise of different members of interdisciplinary team
