12.08 A Day in the Life of Community Falls Teams

Presented by: Iain Wilkinson, Jo Preston, Georgina Gill
Broadcast Date: 1 November 2022
Recording Date: 17 August 2022
Learning outcomes:
Knowledge:
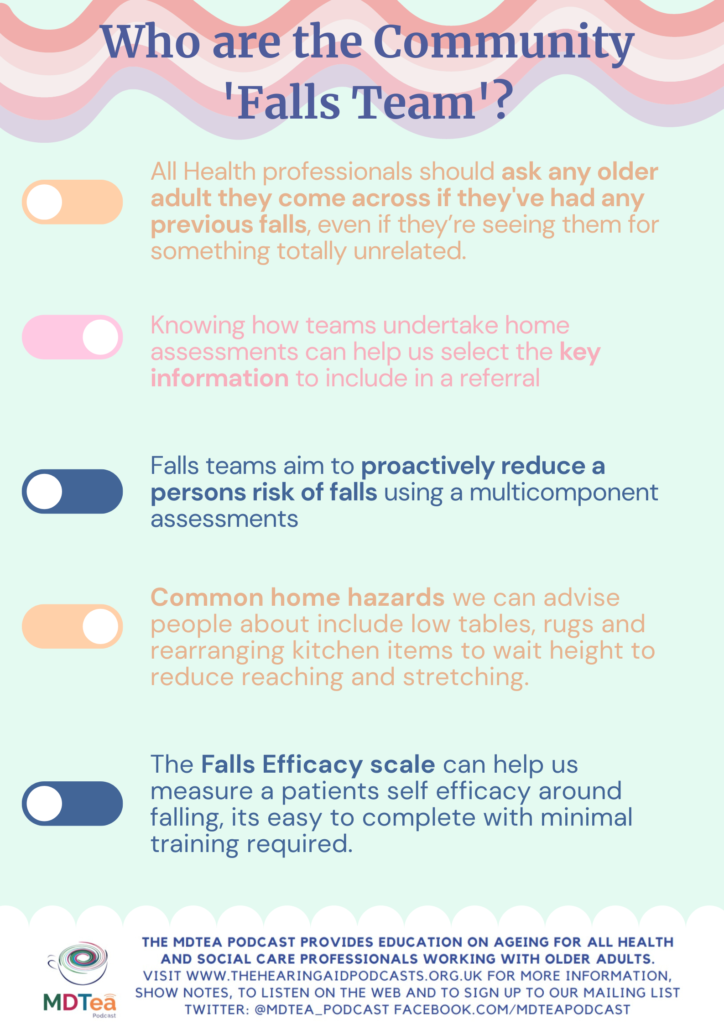
To know the professionals who may make up a community ‘falls team’
To know some of the key assessments and interventions a falls team assessment may utilise.
Skills:
To know the information falls teams may require when receiving a referral
Attitudes:
Consider how we complete referrals to provide onward teams with an appropriate amount of information which avoiding information duplication.
An innovative scheme, which started this month, will see patients who are more at risk of falling given a pair of yellow socks and a yellow blanket so that they are more identifiable to staff, who can better support them 🧦💛
— University Hospitals of Derby and Burton NHS FT (@UHDBTrust) August 10, 2022
Find out more ➡️ https://t.co/vaQlQMofIs pic.twitter.com/q9EjEDMnGg
Paper of the Week
Myrsep A and D Thomson. 2018. Housebound patients’ experiences of a falls service provided by a team of community physiotherapists.
International Journal of Therapy and Rehabilitation, 2018. Vol 25, Iss 12.
- Qualitative descriptive approach to evaluate falls service
- ‘to encapsulate the thoughts, beliefs and feelings of the recipients of this service’.
- Drawn from sample referred by GP, purposeful sampling – to select individuals who were able to purposefully inform an understanding of the research question.
6 housebound participants.
- Interviewed 45 min in own homes using open questions, with probing, rephrasing and summarising, transcripts reviewed by the participants.
- .
inductive process of analysis, thematic analysis
- Generated 4 main themes- the falls, the physiotherapy service, exercise and outcome of the service.
- Included final theme map in article
The Falls
The level of concern about falling among the participants did not consistently match their apparent level of function.
The Physiotherapy Service
- Although some were aware that the physiotherapist was visiting because they had fallen over, nobody mentioned that one purpose was to improve their balance.
Exercise
- Exercises included leg strengthening exercises and balance exercises that are in accordance with NICE (2013) guidelines.
- All the participants believed that exercising was beneficial and can help with movement and reduce pain. One of the participants believed that exercise had to be done regularly for it to be beneficial.
The outcome of the service
They participants said they appreciated the support that the service offered and some achieved improved movement. One participant who had been bedbound was able to walk in his flat and another said his walking had improved.
- Demonstrates improvements in patient outcomes from community physiotherapy services but care is fragmented and often other risk factors not addressed – clinicians need to consider whole picture.
- Recommend an MDT approach for this client group- like the Frailty Teams we met in episode 12.5!
- The authors suggest people who have fallen should be able to refer or re refer themselves to services- suggest improves Service user – Service provider relationship, autonomy and possible improved outcomes.
In order to identify patients who may benefit from falls referral and assessment NICE guidance recommends that all health professionals proactively ask patients about falls at all interactions.
Previous research has shown that participants felt that falls were an inevitable part of ageing and could not be avoided. They were also worried about the consequences of falls, and many did not report falls to health professionals despite being at risk of severe falls in the future. So by asking people about falls we have the opportunity to show them falls can be prevented, are not just an expected part of ageing and provide patients opportunities for referral.
FRAX score, which estimates the 10 year risk of osteoporotic fracture. Factors that the score includes are country of residence, age, sex, race, weight, height, BMI, history of fragility fracture, family histroy of osteoporosis, current smoking history, corticosteroid use, rheumatoid arthritis, secondary osteoporosis and alcohol use.
If using an online calculator the output will be the percentage risk of fracture in 10 years. The national osteoporosis guideline group recommends both supplementation of calcium and vitamin D, and also strongly recommends strength and balance training to those identified to be at risk of falls.
By doing this assessment, teams can identify those who might need a GP to prescribe medications and also who may benefit from referral to local strength and balance classes that the team provide.
HOME Fast Assessment is a screening tool to help those assessing people in their homes to identify key risk factors.
Falls efficacy scale is a scoring tool to help us quantitatively assess a persons fear of falling. Falls self efficacy refers to personal beliefs in one’s ability to engage in certain activities of daily living without falling or losing balance. fear of falling may be an important barrier to consider, as it is associated with distress, increased use of medication, decreased physical function, increased risk of falls, reduced quality of life, activity restrictions, fractures, and admission to institutional care.
Sometimes seeing someone in their own home as opposed to a clinical environment can help professionals assessing them see how people really move and behave which might help us identify risk factors for falling we might not have seen before.
Work by Morrow, Markivics and Harris identified that assessment in the patients own home enabled faster identification of the mechanism of a fall. Advance physiotherapy practitioners delivering home assessment to patients reduced the referral to Geriatricians, and although the rate of readmission with falls increased the number of fractures reduced. The wait time to be reviewed also reduced from 69 days to 20 days.
There’s obviously pros and cons to this approach, and it would be beneficial to know the full range of assessments used by these teams, but reducing the time to assessment is likely to be beneficial as is the benefit of assessment at home. However I read this and thought that maybe its not necessarily benefit to reduce referrals to geriatricians globally and we need to evidence we’re reducing ‘inappropriate’ referrals?
Morrow. Markivics and Harris Poster Presentation, 2022. Pg 13.
What information should we include when making a referral to Falls Team services?
Type of accommodation, number of stairs, is there a lift or stair-lift?
Does the person live alone? If no- who do they live with?
What is property access like? Are there steps, a key safe or care line button?
Has the person had previous fractures? Do they have hearing or vision impairment?
Does the person go outside or are they housebound?
Do they drink alcohol or smoke?
Do they take more than 4-6 medications per day?
What is their medical history do they have any conditions that may increase their risk of falls such as stroke,, Parkinsons or MS?
Do they have any history or low mood, depression or loneliness which might impact their self efficacy?
Overall when referring your patients it useful to take the time to complete referral documents thoroughly to ensure we’re providing the onward teams with sufficient information to make decisions regarding prioritising patients and start considering interventions that might be suitable.
Curriculum Mapping
NHS Key Skills Framework
| Core
Health and Wellbeing | Communication 2:
Personal and People development:
Quality
HWB4 Level 2
HWB4 Level 3
| Communicate with a range of people on a range of matters
Contribute to own personal development
Maintain the quality of own work
Enable people to meet ongoing health and wellbeing needs.
Plan , deliver and evaluate care to meet peoples health and wellbeing needs |
Foundation training Curriculum |
Foundation Year 1 |
Section 2.6 Interface with HCPs
Section 2.7 Interaction with Collegues Section 4:20 Healthcare resource management |
Describes the structure and importance of the wider healthcare team
Works effectively within the healthcare team for the benefit of patient care
Makes clear, concise and timely written and oral referrals to other healthcare professionals within the hospital
Acts as a member of the multidisciplinary professional team by supporting, respecting and being receptive to the views of other healthcare professionals
Works effectively with others towards a common goal e.g. accepts instructions and allocation of tasks from seniors at handovers and multidisciplinary team meetings
Demonstrates understanding of the organisational structure of the NHS and independent sector and their role in the wider health and social care landscape
Describes hospital and departmental management structure
|
Foundation Year 2 |
Section 2.6 Interface with other healthcare professionals
Section 2.7 Interaction with Colleagues
|
Demonstrates ability to make referrals across boundaries / through networks of care (primary, secondary, tertiary)
Demonstrates initiative e.g. by recognising work pressures on others, providing support and organising / allocating work to optimise effectiveness within the clinical team | |
Section 2.7: continuity of care/ Interaction with colleagues
| |||
GP training Curriculum | | Clinical management
Managing complex and long term care
Working with colleagues and in teams
Working well in organisations and systems of care
Community orientation | Contribute to an organisational and professional approach that facilitates continuity of care (e.g. through adequate record keeping and building long term patient relationships)
Organise follow up of your patients after referral through multiprofessional, team bases and structured approaches including monitoring, reviewing and regular care planning.
Demonstrate the ability to effectively ‘navigate’ patients with multiple problems along and between care pathways, enabling them to access appropriate team members and services in a timely and cost-effective manner.
Enhance working relationships by demonstrating understanding, giving effective feedback and maintaining trust.
Appropriately seek advice from other professionals and team members according to their roles and expertise.
Show commitment to a process of continuing professional development through critical reflection and addressing of learning needs.
Recognise the importance of distributed leadership within health organisations, which places responsibility on every team member and values the contribution of the whole team
Describe the current structure of your local healthcare system, including various role, responsibilities and organisations within it, applying this understanding to improve the quality and safety of care you provide.
|
Core medical training curriculum | Managing long term conditions and promoting patient self care: | Define the role of rehabilitation services and the multi-disciplinary team to facilitate long-term care
Recognise importance of multi-disciplinary assessment
Contribute to effective multi-disciplinary discharge planning
| |
Internal medicine training curriculum (Stage 1) | Cat 2.3 . Communicates effectively and is able to share decision making, while maintaining appropriate situational awareness, professional behaviour and professional judgement | Communicates effectively with clinical and other professional colleagues
Applies management and team working skills appropriately, including influencing, negotiating, re- assessing priorities and effectively managing complex, dynamic situations
| |
Geriatrics and higher specialty training curriculum |
30: Rehabilitation and Multidisciplinary team working
31: Planning transfers of Care including discharge | Define the role of rehabilitation services and the multi-disciplinary team to facilitate long-term care
Roles and expertise of different members of interdisciplinary team
Physical therapies which improve muscle strength and function
Therapeutic techniques/training to improve balance and gait
Aids and appliances which reduce disability.
Understand the structure, roles and responsibilities of the multi-disciplinary team including the importance of outside agencies, and the way in which individual behaviours can impact on a group
Role of the geriatrician and the multidisciplinary team in discharge planning |
