12.3 General Practice
Presented by: Iain Wilkinson, Jo Preston and Stephen Collins
Special Guests: Dr Adam McClintock and Alice Poots
Broadcast date: 23rd August 2022

Learning Outcomes
Knowledge:
- To understand what day-to-day life is like in a GP surgery, and what kinds of services they offer to older adults in the community.
- To know the roles played by different healthcare professionals within each GP practice, including doctors, nurses, and other healthcare and administrative staff.
Skills:
- To learn the skills and expertise provided by each member of GP practice staff, and how this contributes to overall, ongoing patient care.
- To appreciate the number of people working behind the scenes in any GP practice in order to keep the whole service functioning as efficiently as possible (from triage staff to receptionists to practice nurses to pharmacists etc).
Attitudes:
- To provide an accurate portrayal of what goes on in a typical day at a GP surgery, and dispel any myths that circulate in the mainstream media about what goes on within these teams.
- To understand why GP’s are busier than before, and what has caused them to be more booked up than ever before.
- To gain an appreciation for the role played by GP’s and their staff in caring for older adults, and to appreciate the challenges they face in their day to day work.
- To hear answers to the public’s questions from the people working in these practices, and to facilitate respectable discussion about what could be done to improve attitudes and overall care of older adults in the community moving forwards.
Paper of the Week
Murphy et al, Implementation of remote consulting in UK primary care following the COVID-19 pandemic: a mixed-methods longitudinal study, British Journal of General Practice (2021), https://bjgp.org/content/bjgp/71/704/e166.full.pdf
Some facts about general practice
- There are around 9,000-10,000 active general practices in the UK today.
- In the GP Patient Survey 2022, with 720,000 responses from patients all over England, 72% of people said they had a “good” experience of their general practice and 91% said their needs were met at their last appointment.
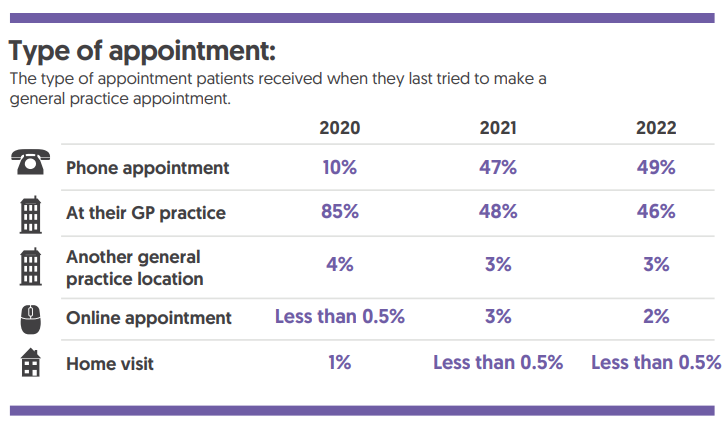
- The same study (accessible at www.gp-patient.co.uk) showed the different types of appointments given to patients over the past 3 years, and gives an idea of how things have changed since before the Covid-19 pandemic:

How might general practice help Jean?
- Jean could attend a hypertension clinic with a practice nurse like Alice (featured in this episode), who might identify that Jean’s blood pressure is high, and organise for Jean to see the GP the following day.
- Then on review with the GP (such as Adam in today’s episode), they might pick up on other things going on in the background with Jean. He might come to realise that Jean has got elevated BP because she’s been forgetting to take her antihypertensive medications as her memory and cognitive function have gradually been declining.
- The GP may recognise that Jean’s becoming increasingly frail and multimorbid, and could calculate this using the electronic frailty index (eFI) score, and think about doing other frailty screening for her and involving other members of the GP team to help better support Jean at home.
- It’s important to ask “What is the right person-centred care for Jean?” as phone or virtual consultations may be more appropriate for some reviews. It might be a huge strain for Jean to get her son to come over, to help get her out of the house and onward to the GP. If her son is able to support a telephone consultation, he could record Jean’s BP at home, and this might even be more accurate if she’s not had the stress of exerting herself in getting to the GP surgery.
- Perhaps in the future, GP’s could consider sending out questionnaires before telephone or virtual appointments so patients have more information at hand when the call takes place, and other family members could also contribute to these questionnaires in advance of the appointed slot. Virtual consultations will be a big part of healthcare moving forward for all of us, so it’s important that we think about how to optimise these on the patient’s behalf.
Social Media this week...
Stephen: Really thought-provoking piece from Emma Ladds in the June 2022 edition of the British Journal of General Practice, entitled “Recognising the value of a bunch of tulips in general practice” highlighting the importance of human interaction and empathy in primary care despite the inevitable challenges and stresses of the job.
NHS Key Skills Framework
Core
Develop and maintain communication with people on complex matters, issues and ideas and/or in complex situations
Health and Wellbeing
Plan, deliver and evaluate interventions and/or treatments
Prepare and supply specialised products
Foundation Curriculum (Year One and Year Two)
1.2 Patient centred care
Works with patients and colleagues to develop individual care plans
2.6 Communicates clearly in a variety of settings
Works effectively within the healthcare team for the benefit of patient care
Makes clear, concise and timely written and oral referrals to other healthcare professionals within the hospital
2.7 Works effectively as a team member
Acts as a member of the multidisciplinary professional team by supporting, respecting and being receptive to the views of other healthcare professionals
3.10 Recognises, assesses and manages patients with long-term conditions
Recognises frailty
Formulates individual patient management plan based on assessment of frailty as well as clinical need
3.11 Obtains history, performs clinical examination, formulates discharge planning
Liaises and communicates with the patient, family and carers and supporting teams to arrange appropriate follow up
3.17 Manages palliative and end of life care
Participates in discussions regarding personalised care planning including symptom management and advance care plans with patients, family and carers
GP Training Curriculum
Communication and consultation
Have appropriate communication skills for counselling, teaching and treating patients, their families and carers, and recognising the difficulties of communicating with older patients
Making decisions
Recognise the importance of a problem-based approach, taking in the ‘big picture’, rather than a disease-based approach to the care of older people, who often have complex physical, psychological and social problems
Clinical management
Know how to access support services for older patients, e.g. podiatry, visual and hearing aids, immobility and walking aids, meals on wheels, home care services
Ensure that the provision of care promotes the patient’s sense of identity and personal dignity, and that the patient is not discriminated against as a result of their age
Managing medical complexity
Understand how co-morbidity will influence the management of existing disease and delay the early recognition of adverse clinical patterns
Core Medical Trainee
- Common competencies:
Managing patient conditions and promoting patient self-care
Outline the concept of quality of life and how it can be measured
- Geriatric medicine competencies:
Understand the factors which influence health – psychological, biological, social, cultural and economic especially work and poverty
Internal Medicine Training Curriculum
Generic CiP3:
Communicates effectively and is able to share decision making, while maintaining appropriate situational awareness, professional behaviour and professional judgement
Geriatrics and Higher Specialty Training Curriculum
- Rehabilitation and Multidisciplinary Team Working
Principles of rehabilitation and comprehensive assessment
Roles and expertise of different members of interdisciplinary team
