11.9 A Day in the Life of a Dietitian
Presented by: Iain Wilkinson, Stephen Collins, Georgie Gill
Special Guests: David Gray and Lorna King
Broadcast date: 3rd May 2022
Learning Outcomes
Knowledge:
- To know the role played by dietitians and see the crucial role they play in helping patients maintain a nutrient-rich diet into older age.
- To understand why older adults are often prone to malnutrition, and what can be done to address this.
- To recognise the importance of placing a patient’s own tastes at the centre of dietary decision making, and ensuring that the food and nutritional supplements you are giving them are enjoyable and something they are willing to take.
Skills:
- To learn how dietitians use methods such as food fortification to enhance the diets of certain older adults, as a way of boosting nutritional intake.
- To understand the components of a healthy, nutrient rich diet, and to know what foods to suggest to older adults for them to meet their nutritional requirements each day.
Attitudes:
- To gain a fresh appreciation for the role played by dietitians in improving the quality of life in older adults and helping them grow in energy and strength in a way that significantly aids their rehab in hospital.
- To recognise that nutritional supplements are not a long-term fix, but rather a short-term means of bridging the gap when a patient is noted to have a nutritional deficit.
- To see how valuable food charts are when it comes to physical examination of a patient on the ward. So much important information can be gained from seeing what a patient has managed to eat and drink in the past 24 hours!
Stephen: Joe Middleton (@_JoeMiddleton) – “Mobility is a vital sign”
Mobility is a vital sign.
— Joe Middleton (@_JoeMiddleton) April 25, 2022
A new deterioration in mobility is an important clinical sign of physical/functional/cognitive decompensation to an acute stressor. https://t.co/Z29NwejnA7
Key Learning Points about Dietitians
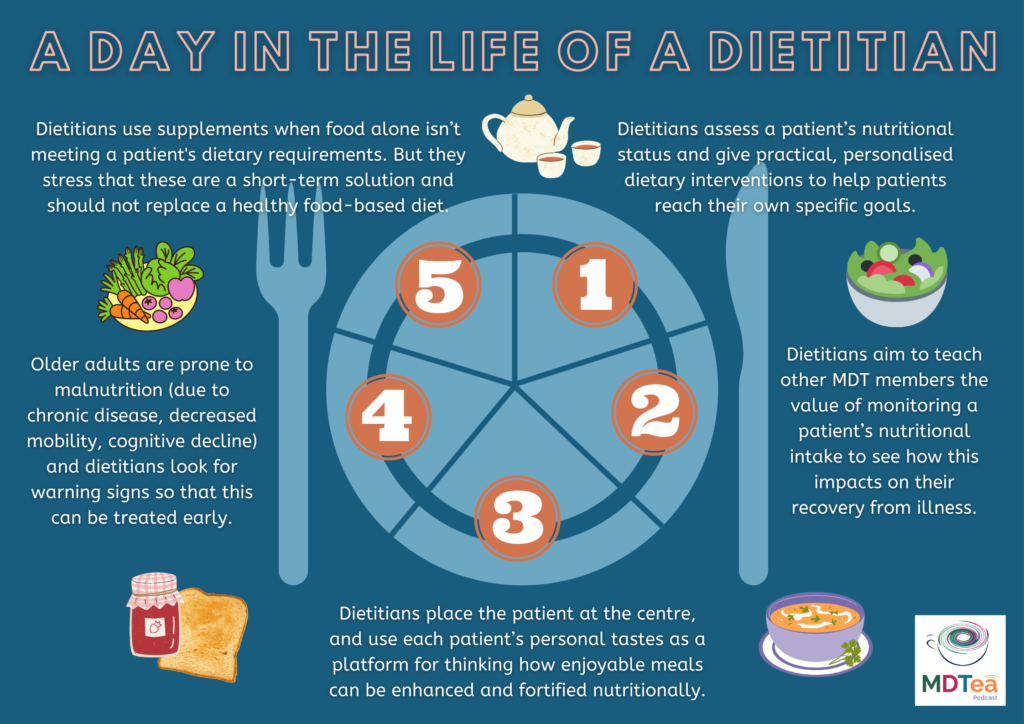
1) The role of a dietitian focuses on assessing a patient’s nutritional status and give practical, personalised dietary interventions to help a patient reach their specific goals.
2) Dietitians work closely with other members of the hospital MDT, and aim to teach other healthcare professionals to see the value of closely monitoring a patient’s nutritional intake and see how this impacts on their recovery and ongoing health and wellbeing.
3) Dietitians place the patient at the centre of their decision-making when drawing up diet plans, and aim to use the patient’s personal tastes as a platform for thinking about how certain enjoyable meals could be enhanced and fortified nutritionally.
4) Older adults are more prone to malnutrition than their younger counterparts for a number of reasons, and dietitians are experienced in detecting any warning signs that suggest that an older patient may need dietary interventions to prevent further health complications down the line.
5) Dietitians use supplements in their management plans, but only as a short-term bridge. They appreciate the benefit of supplements in boosting a patient’s diet during recovery from illness or when food alone isn’t meeting their dietary requirements, but all dietitians stress that supplements are not a long-term solution, and shouldn’t be seen as such.
Some facts and figures about dietitians
There are over 9000 Dietitians registered in the UK, an increase of almost 50% in the last decade. The profession is carrying out extended roles that were unthinkable 10 years ago and have introduced new roles such as dietetic support workers, assistant practitioners and nutritionists to the workforce.
The BDA, founded in 1936, is the professional association and trade union for dietitians in Great Britain and Northern Ireland. It is the nation’s largest organisation of food and nutrition professionals with over 7,500 members.
Dietitians translate nutrition science into understandable, practical information about food, allowing people to make appropriate lifestyle and food choices, they treat a range of medical conditions with dietary therapy specially tailored to each individual, and they advise on healthy eating for all ages, races, cultures and social groups.
Useful Definitions
Food fortification= Fortification is the practice of deliberately increasing the content of one or more micronutrients (i.e. vitamins and minerals) in a food or condiment to improve the nutritional quality of the food supply and provide a public health benefit with minimal risk to health.
The term can also refer to the addition of extra elements to a patient’s meals in order to boost their calorie content, such as in the cases of frail, older people having double cream or cheese added to their everyday meals.
Dietary Protein in the Elderly=
- The recommended dietary protein for adults is 0.8 g/kg/day. However, this value does not take into account the requirements for populations (like the elderly) who may reap additional health benefits, particularly for skeletal muscle, from higher dietary protein intake.
- Protein is particularly important for delaying frailty and maintaining muscle mass and function

How would the dietitians help with Jean?
Keep in mind her Parkinson’s disease, and monitor closely how that affects her appetite/diet. They would also watch for any change in her swallow, to know if the consistency or texture of her diet needs altered.
Consider which foods might best build up her strength again during her rehab and recovery. They may suggest short-term dietary supplements in addition to her food to help bridge the gap with her nutritional deficit.
Aim to provide a familiar and enjoyable diet, given Jean’s history of dementia, and they would look to enhance and fortify her own favourite foods, as a way of boosting her nutritional intake.
#MDTeaser

Curriculum Mapping
NHS Key Skills Framework
Core
Develop and maintain communication with people on complex matters, issues and ideas and/or in complex situations
Health and Wellbeing
Plan, deliver and evaluate interventions and/or treatments
Prepare and supply specialised products
Foundation Curriculum
Year One and Year Two
1.2 Patient centred care
Works with patients and colleagues to develop individual care plans
2.7 Works effectively as a team member
Acts as a member of the multidisciplinary professional team by supporting, respecting and being receptive to the views of other healthcare professionals
Works effectively with others towards a common goal e.g. accepts instructions and allocation of tasks from seniors at handovers and multidisciplinary team meetings
3.10 Recognises, assesses and manages patients with long-term conditions
Formulates individual patient management plan based on assessment of frailty as well as clinical need
GP Training Curriculum
Communication and consultation
Have appropriate communication skills for counselling, teaching and treating patients, their families and carers, and recognising the difficulties of communicating with older patients
Making decisions
Recognise the importance of a problem-based approach, taking in the ‘big picture’, rather than a disease-based approach to the care of older people, who often have complex physical, psychological and social problems
Clinical management
Understand the physical factors – particularly diet, exercise, ambient temperature and sleep – that disproportionately affect the health of older people
Know how to access support services for older patients, e.g. podiatry, visual and hearing aids, immobility and walking aids, meals on wheels, home care services
Ensure that the provision of care promotes the patient’s sense of identity and personal dignity, and that the patient is not discriminated against as a result of their age
Core Medical Trainee
- Common competencies:
Managing patient conditions and promoting patient self-care
Outline the concept of quality of life and how it can be measured
- Geriatric medicine competencies:
Understand the factors which influence health – psychological, biological, social, cultural and economic especially work and poverty
Internal Medicine Training Curriculum
Generic CiP3:
Communicates effectively and is able to share decision making, while maintaining appropriate situational awareness, professional behaviour and professional judgement
Geriatrics and Higher Specialty Training Curriculum
- Rehabilitation and Multidisciplinary Team Working
Principles of rehabilitation and comprehensive assessment
Roles and expertise of different members of interdisciplinary team
Reference List
American Parkinson’s Disease Association, Weight Loss and Parkinson’s Disease, 2019, https://www.apdaparkinson.org/article/weight-loss-parkinsons-disease/
BDA (British Dietetic Association), What is a dietitian? 2017, https://www.hct.nhs.uk/media/1083/what-is-a-dietitian.pdf
BDA, Workforce, https://www.bda.uk.com/practice-and-education/nutrition-and-dietetic-practice/professional-guidance/workforce.html
Breen and Smeuninx, Dietary protein recommendations for the elderly, Milk and Dairy Foods, 2020, https://www.sciencedirect.com/topics/agricultural-and-biological-sciences/dietary-protein
NHS Central London Community Healthcare, Food Fortification, 2010, https://www.rbkc.gov.uk/pdf/food%20fortification.pdf
University of Sheffield, Association between low protein and increased frailty, 2020, https://www.sheffield.ac.uk/news/nr/healthy-lifespan-consume-protein-stay-healthy-1.881651
World Health Organisation, Food fortification, https://www.who.int/health-topics/food-fortification#:~:text=Fortification%20is%20the%20practice%20of,with%20minimal%20risk%20to%20health
