11.5 A Day in the Life of a Physician Associate
Presented by: Iain Wilkinson, Stephen Collins and Georgie Gill
Contributors: James Catton, Lindsay Nelson, Mira Pun and Hamed Rohani
Learning Outcomes:
Knowledge:
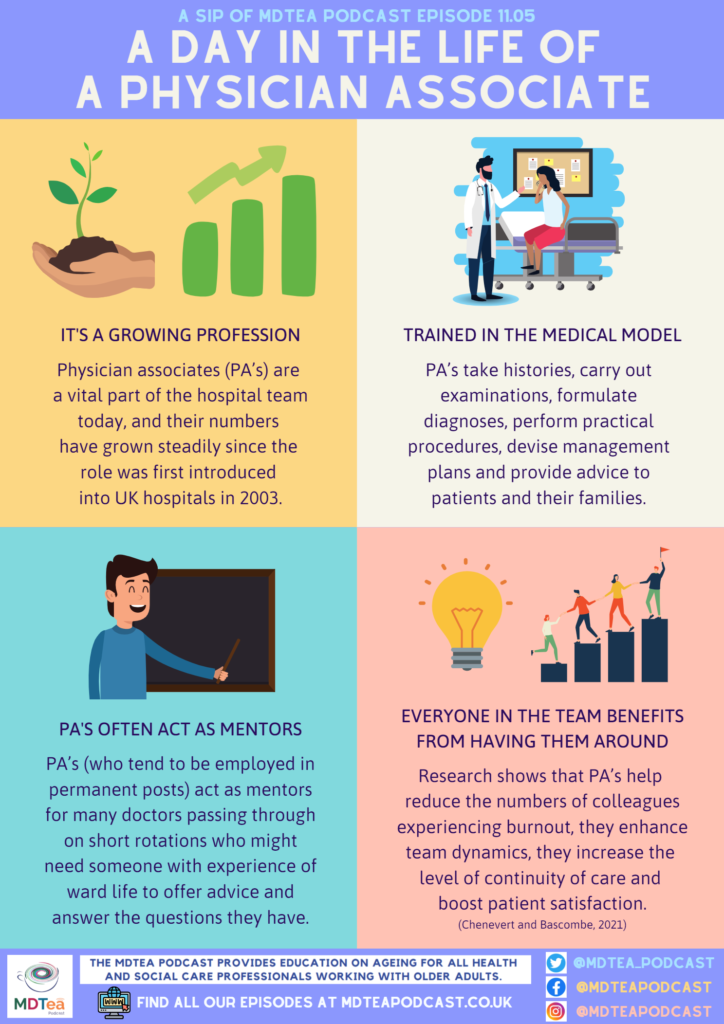
– To develop an understanding of who physician associates are, and what
role they play within the hospital MDT
– Recognise that, while it is a relatively new profession in the UK, it is
rapidly growing and lots more PA’s are qualifying every year after being
trained in the medical model.
– Consider the breadth of the PA role, from complex practical procedures
and assessing patients right through to taking on leadership roles and acting
as mentors for junior doctors arriving on the wards.
Skills:
– Improve our ability to work as an effective MDT by gaining an
appreciation for the full skill set that is on offer from the many PA’s working
in our hospitals.
– Know the responsibilities that PA’s can take on (reviewing patients and
forming management plans), and talk with them and ask for their advice as they
often form close relationships with patients and their families due to the more
permanent nature of their role.
Attitudes:
– Challenge assumptions that some doctors may have about where PA’s fit into a medical team, by helping them understand the medical training PA’s have and their willingness to help with the assessment of management of unwell patients.
– Gain an appreciation of how PA’s are part of a fresh, exciting approach to hospital medicine, and see how we can learn from them and encourage them in the fantastic work they do.
Social Media
Stephen: “Prescribing cascades” – as mentioned by the Twitter account @pharmacopallia. Talking about how more and more meds are often added, without seeing if rationalising might reduce the medication burden and prevent new problems from arising.
https://twitter.com/pharmacopallia/status/1495037253516763139
Iain: Article in the Guardian re: Clare Gerada, and her reflections on how GP work has changed over the course of three decades in the job.
Definitions
Physician Associate= healthcare professionals with a generalist medical education. They are trained in the medical model, and function under the supervision of a doctor. In their role, they take patient’s medical histories, perform examinations, make diagnoses, request tests, analyse results and initiate treatment.
Voluntary register= Physician Associates in the UK are not currently a mandatory regulated profession. They have a voluntary register which is managed by the Faculty of Physician Associates (FPA) as part of the Royal College of Physicians (RCP), and will continue to do so until they are granted formal recognition and regulation by the General Medical Council.
GMC Regulation= Professional regulation means the people who work within a particular profession are regulated to ensure they are fit to practice. Being regulated ensures everyone in that profession has received a certain level of education/training, fulfil certain criteria and are competent at their jobs. GMC regulation would mean that the organisation would have responsibility and oversight of all physician associates.
Ionising radiation= This includes imaging such as X-rays and CT scans. Ionising radiation has more energy than non-ionising radiation, enough to cause chemical changes by breaking chemical bonds. This effect can cause damage to living tissue, and this is why PA’s need to await formal regulation before they are permitted to request scans of this kind.
Some facts and figures about PA's today...
- The role of physician associate has been an integral part of the US healthcare workforce since the 1960s but is relatively new in the UK.
- Initial training programmes for small numbers of physician associates were first set up in the UK in 2004. There are now 36 programmes across the UK, and more than 1000 students graduate every year.
- The number of physician associates (PA’s) training and working in the UK has increased over the last few years following the proliferation of postgraduate courses.
- Physician assistants/associates are trained in the generalist medical model and function under the supervision of a doctor.
- Tasks relating to the role include the following: taking patient’s medical histories, performing examinations, making diagnosis, requesting tests, analysing results and the initiation of treatment.
- Physician associates are currently an unregulated healthcare profession but, once qualified, are strongly encouraged to join the physician associate managed voluntary register.
- Once on the register they have to complete 50 hours of continuing professional development annually and pass a re-certification examination every six years.
- Physician assistants in the USA and the Netherlands have prescribing privileges. Statutory regulation for physician assistants/associates lays the groundwork for prescribing privileges and such regulation is under consideration by the government in the UK.
- According to the most recent FPA census of PA’s in the UK, 94% of PA’s say they enjoy their job, and 92% would recommend it to a friend.
- The General Medical Council (GMC) has announced that it plans to formally regulate physician associates in the near future, and this should open the door for PA’s to prescribe and request ionising scans in hospital. It is hoped that this regulation will be passed around Summer 2023 as things stand.

So where is Jean now?
We have been walking with our patient Jean through each step of her hospital journey as we’ve moved through Series 11.
So far we have seen Jean assessed and brought into the hospital by paramedics after a fall and long lie at home. She was reviewed by ED nurses and doctors, before being admitted to a medical ward for further investigations.
On arriving on the ward, she had her medications list looked at closely by the pharmacist, and inappropriate medications were held or stopped.
Now Jean needs daily review by the ward team, and it is quite likely that one of the physician associates might carry out this task. So who are the PA’s that Jean might meet?
What regular interaction do the PA’s featured on this episode have with older patients like Jean?
James:
Works part of his week in a GP surgery and the other half of his week in a hospital acute medical unit. The part of the UK he works in has the 2nd highest elderly population in the UK, and so he sees a lot of frail, older patients like Jean. He says that polypharmacy is one of the biggest issues, and is always looking to reduce the medications burden on patients where possible, as well as doing falls risk assessments to ensure their safety.
Hamed:
Works full-time in a hospital medical assessment unit. He says that when looking after older patients like Jean, one of the most important things to manage is delirium. It can often be difficult to establish the full story from patients who are delirious, and so Hamed works hard to speak to family who can help him understand the patient’s baseline better. He also says that constipation and reduced oral intake can be frequent problems for older patients, and these are things that PA’s like him monitor closely.
Mira:
Works for half of each week as a PA on an elderly care ward, and spends the other half of her week doing a research and quality improvement project looking at the role of ReSPECT forms in advance care planning within the hospital setting. She explains that it can be challenging looking after older patients like Jean with multiple comorbidities, and this level of multimorbidity can result in complex discharge planning. But she finds it very rewarding looking after vulnerable patients with palliative care needs.
Lindsay:
Works as a PA on a busy surgical unit in Northern Ireland. She says that with her older patients, such as Jean, post-operative delirium is the biggest challenge she faces. She explains that surgeons are often not familiar with all of the complexities of delirium management, and this means that Lindsay needs to liaise on a regular basis with medical staff and members of the frailty team and mental health team. She works hard to develop a personal relationship with each of her older patients, and ensures they have someone they can voice their concerns to, as well as making sure they are familiar with the staff and their surroundings to minimise confusion.
Curriculum Mapping
NHS Key Skills Framework
Core
Develop and maintain communication with people on complex matters, issues and ideas and/or in complex situations
Health and Wellbeing
Plan, deliver and evaluate care to address people’s complex health and wellbeing needs
Assess physiological and/or psychological functioning and develop, monitor and review related treatment plans.
Plan, deliver and evaluate interventions and/or treatments
Foundation Curriculum
Year One
1.2 Patient centred care
– Works with patients and colleagues to develop individual care plans
1.3 Mental capacity
– Recognises the potentially vulnerable patient.
– Manages situations where safeguarding concerns may exist.
2.6 Communicates clearly in a variety of settings
– Works effectively within the healthcare team for the benefit of patient care
– Makes clear, concise and timely written and oral referrals to other healthcare professionals within the hospital
2.7 Works effectively as a team member
– Acts as a member of the multidisciplinary professional team by supporting, respecting and being receptive to the views of other healthcare professionals
– Works effectively with others towards a common goal e.g. accepts instructions and allocation of tasks from seniors at handovers and multidisciplinary team meetings
– Gives structured handover to ensure safe continuing care of patients.
3.10 Recognises, assesses and manages patients with long-term conditions
– Recognises frailty
– Formulates individual patient management plan based on assessment of frailty as well as clinical need
– Cares for patients with long-term diseases during their in-patient stay
3.18 Recognises and works within the limits of personal competence
Recognises and works within limits of competency
Foundation Curriculum
Year Two
1.2 Delivers patient centred care and maintains trust
Discusses management options with patients and responds to their ideas, concerns and expectations
2.6 Communicates clearly in a variety of settings
Demonstrates ability to make referrals across boundaries / through networks of care (primary, secondary, tertiary)
3.11 Obtains history, performs clinical examination, formulates discharge planning
– Anticipates clinical evolution and starts planning discharge and ongoing care from the time of admission
– Liaises and communicates with the patient, family and carers and supporting teams to arrange appropriate follow up
3.17 Manages palliative and end of life care
Participates in discussions regarding personalised care planning including symptom management and advance care plans with patients, family and carers
GP Training Curriculum
Fitness to practice
– Recognise your attitudes to the use of intensive or invasive tests and treatments and the use of limited healthcare resources in the care of the elderly
– Be aware of these broader factors in order to counter personal biases that are unhelpful to the care of the elderly
Communication and consultation
Have appropriate communication skills for counselling, teaching and treating patients, their families and carers, and recognising the difficulties of communicating with older patients
Making decisions
– Recognise the importance of a problem-based approach, taking in the ‘big picture’, rather than a disease-based approach to the care of older people, who often have complex physical, psychological and social problems
Clinical management
– Understand the management of the conditions and problems commonly associated with old age, such as Parkinson’s disease, falls, gait disorders, stroke, confusion, dementia and cancer
Managing medical complexity
Understand how co-morbidity will influence the management of existing disease and delay the early recognition of adverse clinical patterns
Core Medical Trainee
- Common competencies:
Managing patient conditions and promoting patient self-care
Recall the natural history of disease that run a chronic course
- Geriatric medicine competencies:
– Recognise when specialist geriatric medicine opinion is indicated
– Recognise importance of multi-disciplinary assessment
– Rationalise individual drug regimens to avoid unnecessary polypharmacy
– Contribute to discussions on decisions not to resuscitate with patient, carers, family and colleagues appropriately, and sensitively ensuring patients interests are paramount
– Recognise that older patients often present with multiple problems (e.g. falls and confusion, immobility and incontinence)
Internal Medicine Training Curriculum
Generic CiP3:
Communicates effectively and is able to share decision making, while maintaining appropriate situational awareness, professional behaviour and professional judgement
Generic CiP6:
Delivers effective teaching and training to medical students, junior doctors and other healthcare staff
Geriatrics and Higher Specialty Training Curriculum
- Comprehensive geriatric assessment
– Recognise that good health includes both physical and mental wellbeing and social, sexual and spiritual aspects
- Diagnosis and management of chronic disease and disability
– The major chronic illnesses and disabling conditions seen in older people
- Rehabilitation and Multidisciplinary Team Working
– Principles of rehabilitation and comprehensive assessment
– Roles and expertise of different members of interdisciplinary team
- Delirium
– Risk factors and causes
– Non-pharmacological management
- Falls
– Causes of and risk factors for falls
- Community practice including Continuing, Respite and Intermediate Care
– End of Life Care including advanced care planning
- Care of older people living with frailty
– Clinical presentation of frail older people
Resources and other useful information...
The FPA Census 2020, Faculty of Physician Associates, https://www.fparcp.co.uk/about-fpa/fpa-census
The physician associate will see you now – new role to assist patients in primary care, NHS England, https://www.england.nhs.uk/gp/case-studies/the-physician-associate-will-see-you-now-new-role-to-assist-patients-in-primary-care/
Physician associates need support to establish their place within the healthcare workforce, National Institute for Health Research, https://evidence.nihr.ac.uk/alert/physician-associates-need-support-establish-place-within-healthcare-workforce/
The early experiences of Physician Associate students in the UK: A regional cross-sectional study investigating factors associated with engagement, Howarth et al, PLoS ONE, 2020, https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0232515
Building the evidence base-10 years of PA research in England, Drennan and Halter, JAAPA, 2020, https://pubmed.ncbi.nlm.nih.gov/32976241/
The role of the physician associate: an overview, Malone, Ir J Med Sci, 2021, https://pubmed.ncbi.nlm.nih.gov/34351601/
GMC publishes future professional standards for PAs and AAs, General Medical Council, October 2021, https://www.gmc-uk.org/news/news-archive/gmc-publishes-future-professional-standards-for-pas-and-aas
Physician associate – regulation update, Faculty of Physician Associates, https://www.fparcp.co.uk/about-fpa/news/physician-associate-regulation-update
Your guide to PA regulation, Not A Doctor, 2020, https://www.notadoctor.co.uk/single-post/your-guide-to-pa-regulation